Cause and Prevention of Common Vein Conditions
What Causes Vein Conditions?

Understanding Different Vein Conditions
Three Types of Vein Conditions
- Varicose Veins
- Spider veins
- Reticular veins
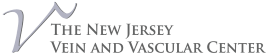
What are Varicose Veins?

Symptom and Causes:
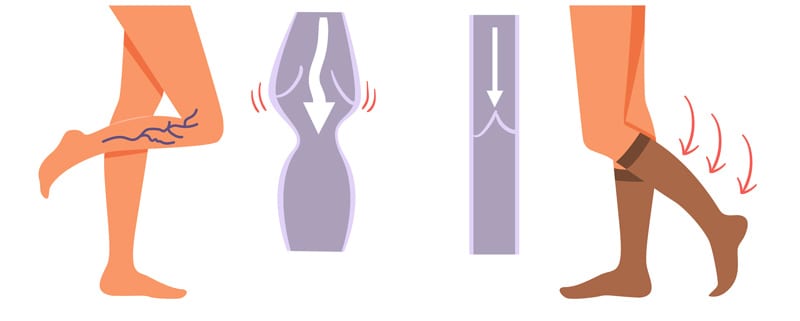
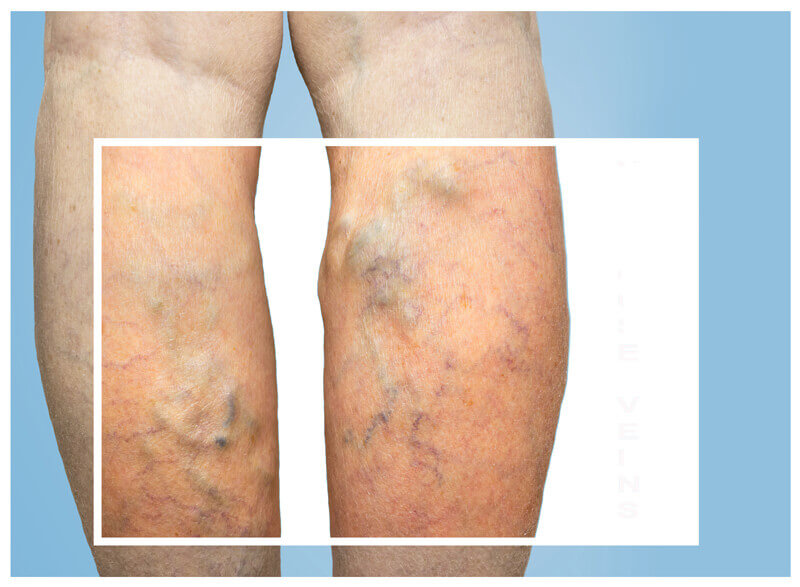
Symptoms of varicose veins include pain in the leg, cramping, continuous fatigue or heaviness in the legs. Other symptoms include swelling in the ankles, restlessness and in more severe cases, blisters and ulcers. There are many factors that can raise the risks of varicose veins according to the National Institutes of Health (NIH). Some of these include family factors such as their history, age, chronic problems, pregnancy, obesity, and lifestyle. People in certain jobs or occupations may develop this condition as well, particularly those who sit/stand for a prolonged period. Varicose veins can be extremely disrupting as it may limit or impair a person’s movement which can affect their quality of life.
What Are Spider Veins?

Symptom and Causes:
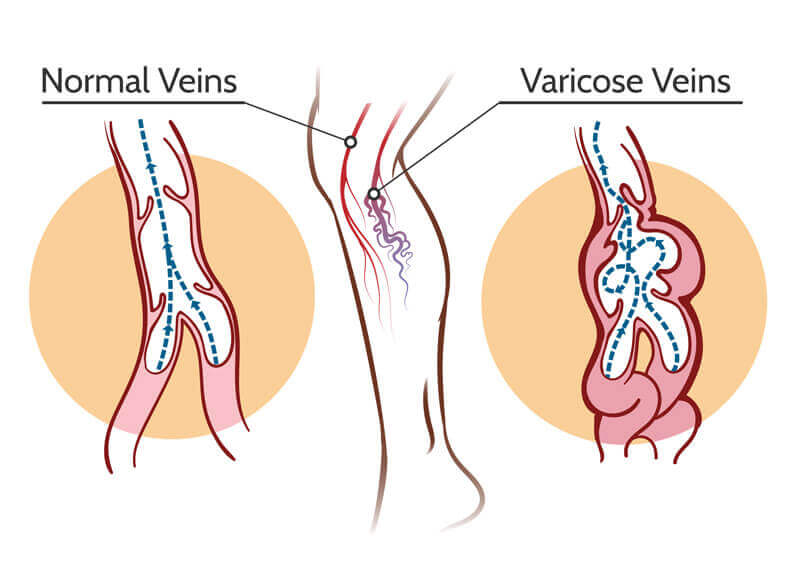
Spider veins may cause itching, burning and even severe discomfort and pain. But, for many people there may be no symptoms present aside from the appearance of veins. Just like in varicose veins, spider veins are also caused by a common medical condition which is known as venous insufficiency. As discussed previously, our veins carry blood from our body tissues to the heart. Our hearts then replenish the blood supply with oxygen and re-circulate it throughout the body. This is made possible with the help of tiny one-way valves. Each vein has microvalves and with every pump of the heart, our blood flows through a series of them in the veins. This is to help the blood flow travel upward from our legs as it returns to the heart. When these valves fail or leak, the blood collects in this region causing the veins to form a spider web-like appearance.
What Are Reticular Veins?

Symptom and Causes:
Reticular veins are very common, affecting about 80% of adults and can be caused by hormone imbalances, weak veins, or as a result of certain genetic factors. It also depends on weight, UV skin damage, and occupations which require a lot of time spent sitting or standing.
Prevention
- Exercise regularly to improve your leg strength, circulation, and vein strength, however, do not overdo it. Exercise should be done in a disciplined manner. Overexerting yourself may put extra pressure on the veins and can cause muscle pain.
- Control your weight to avoid placing too much pressure on your legs. Excessive weight puts a lot of pressure on the veins and can promote venous disease, damaging the veins and cause them to pop out.
- Eat healthy food and maintain a good diet. Adding fruits, vegetables, and vital nutrients can help improve circulation and keep veins healthy.
- Take proper care of your body and skin, maintaining a healthy, active lifestyle and consult a doctor if you feel any leg pain, discomfort, uneasiness or restlessness in your legs.
- Embrace a healthy lifestyle, get rid of unhealthy habits like smoking, excessive drinking or eating too much junk food.
- Do not cross your legs when sitting and try to elevate your legs when resting
- Do not stand for long periods of time
By taking these preventive measures, you can not only maintain healthy circulation and veins but also improve the overall health of your skin and vascular system.