Varicose veins are those unsightly bulging veins that you often see on legs or feet. If you have them, you’re probably aware of the discomfort or pain they can cause—especially after a long day of standing or sitting. Compression therapy...
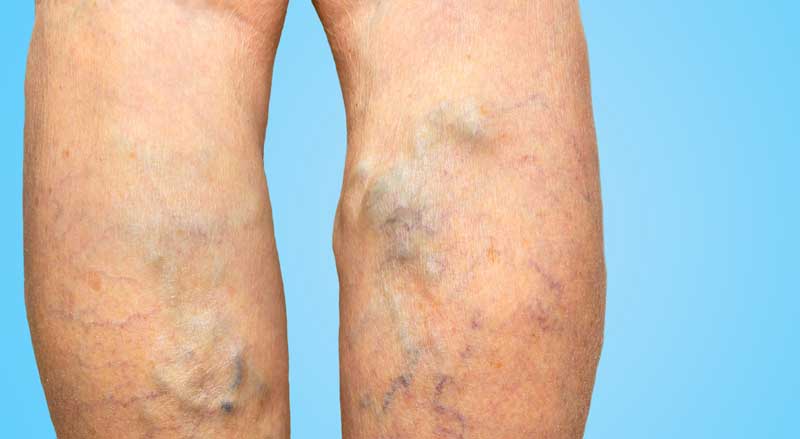
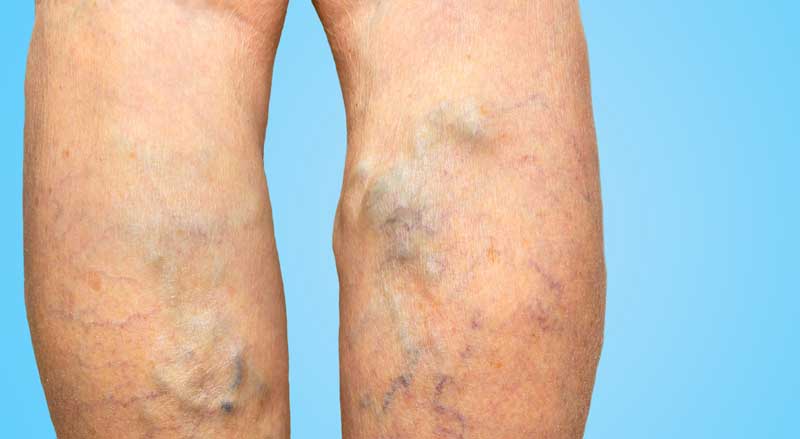
Varicose veins are those unsightly bulging veins that you often see on legs or feet. If you have them, you’re probably aware of the discomfort or pain they can cause—especially after a long day of standing or sitting. Compression therapy...

The state-of-the-art treatment for eliminating unsightly or bothersome veins is sclerotherapy. This popular, minimally invasive treatment is highly effective in reducing the symptoms and appearance of certain veins. But a common question about sclerotherapy is how long does it last?...

Learn the warning signs and why a proper diagnosis of varicose vein disease is so important. Do you get cramps in your legs overnight or have restless legs? Are your legs often itchy for no apparent reason? The cause of...

Did you know knee replacement surgery or treatment of other orthopedic injuries can significantly affect vein health? Or that sometimes, varicose vein problems can be the actual cause of knee pain? Here’s information about orthopedic surgery and varicose veins—what you...

Most people know the difference between spider veins and varicose veins. But what about spider veins vs. reticular veins? What’s the difference? Veins are the structures that bring blood up from your legs and back to your heart. Three major...

There’s an old saying, “You are what you eat.” This is particularly true for vein health. If you have been wondering about diet and varicose veins, you’ll be interested to learn what’s the connection. While a great diet can’t remove...