Some foods make more of an impact on vein health than others. That is why we have compiled a list of the best power foods to eat for your circulation.


Some foods make more of an impact on vein health than others. That is why we have compiled a list of the best power foods to eat for your circulation.

Spider veins are small veins that appear in clusters, resembling spiderwebs or tree branches. While spider veins are not a medical concern, many individuals treat them for cosmetic reasons. Are you wondering why you are suddenly seeing spider veins? Find...

Do your legs feel achy or stiff at the end of the day? Do you experience unexplained leg pain? If you haven’t made any substantial changes to your daily routine, or if you’re getting older, circulation health could be to...
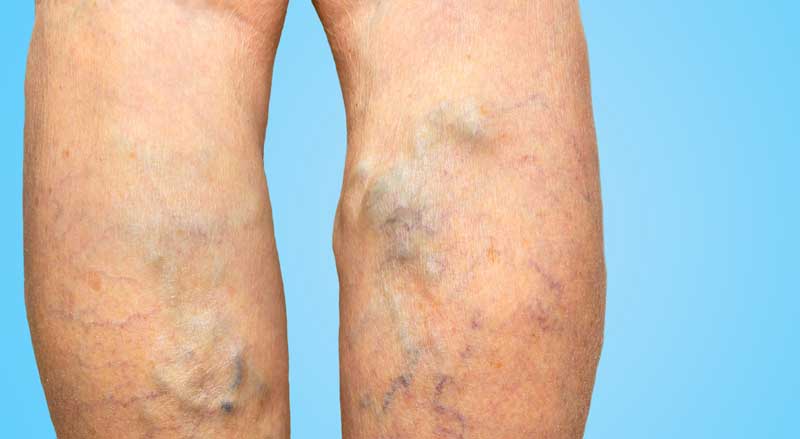
Varicose veins are those unsightly bulging veins that you often see on legs or feet. If you have them, you’re probably aware of the discomfort or pain they can cause—especially after a long day of standing or sitting. Compression therapy...

Poor circulation can affect many areas of your body, including your legs, feet, and toes. There are many reasons for poor blood circulation in the legs and feet, and usually several things you can do to improve your circulation. It’s...
Traveler’s thrombosis, also known as economy class syndrome or deep vein thrombosis (DVT), is a medical condition that can occur when a blood clot forms in a deep vein, usually in the leg, after prolonged periods of sitting, such as...