The Effects of Sleep on Your Health
How well did you sleep last night? If you didn’t get a full seven or eight hours, you aren’t alone. About one-third of adults get less sleep than recommended, according to the Centers for Disease Control and Prevention. It’s important to understand the effects of sleep on your health.
Bouncing between work, family, friends, and responsibilities can leave very little time for rest. However, when you don’t get your daily recommended dose, you are putting your routine and health at risk.
Sleep and Your Immune System

Everyone knows that sleep is important for both mental and physical recovery. Without the proper amount of rest, your body is in danger of infection and disease.
When you choose to stay up over going to bed, your body starts to produce fewer cytokines. Cytokines are essential proteins that promote sleep. These proteins are very important when you’re sick, as the body needs more rest.
Studies have shown that when your body is sleep deprived you are more susceptible to infection. Even coming into contact with simple viruses such as the common cold puts you at risk of becoming very ill.
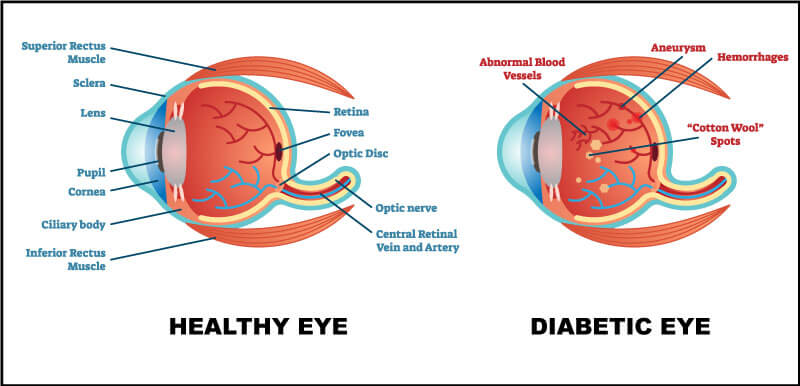
Long-term and serious problems from lack of sleep include diabetes, hypertension, heart attack, stroke, obesity, depression, and lower sex drive.
Sleep and Your Personal Life
There are many short-term effects from lack of sleep that can occur even when missing as little as 1.5 hours. These effects include lowered alertness and the inability to remember and process information.
Surprisingly, scientists have stated that when we sleep our memory may be emptying unneeded knowledge. It does this to free up space for new information and memories we make in the future. Without clearing this knowledge, it’s difficult for us to grasp new information.
Being able to properly process what you are being told, whether it’s at work or school, is important for keeping your job or maintaining a good GPA. Lack of sleep can also make you moody and more likely to have conflicts with family and co-workers.
Sleep and Your Veins and Arteries
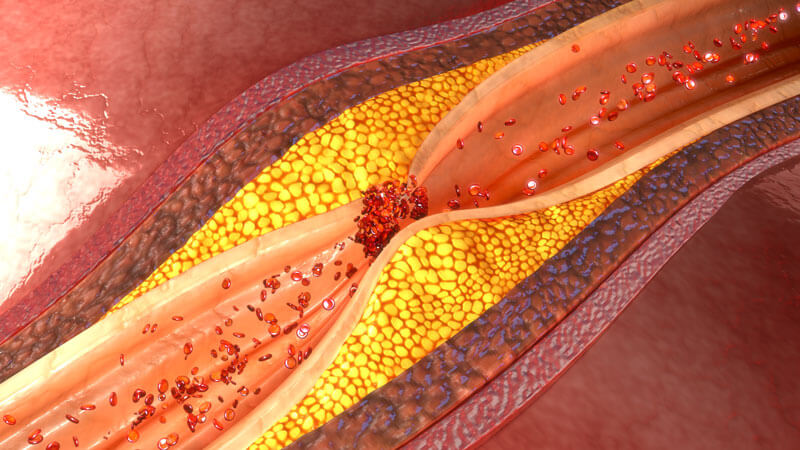
According to research recently reported by Science News, people who do not get enough sleep have lower levels of good cholesterol. Sleep usually protects your arteries by removing bad cholesterol.
When bad cholesterol isn’t removed, it builds up in your arteries causing heart disease. Atherosclerosis, a condition caused by plaque buildup in the arteries, increases the risk of heart health issues and stroke.
Just one week of fewer hours of sleep changes your immune responses and metabolism. The metabolic processes needed to keep good cholesterol flowing through the body is affected.
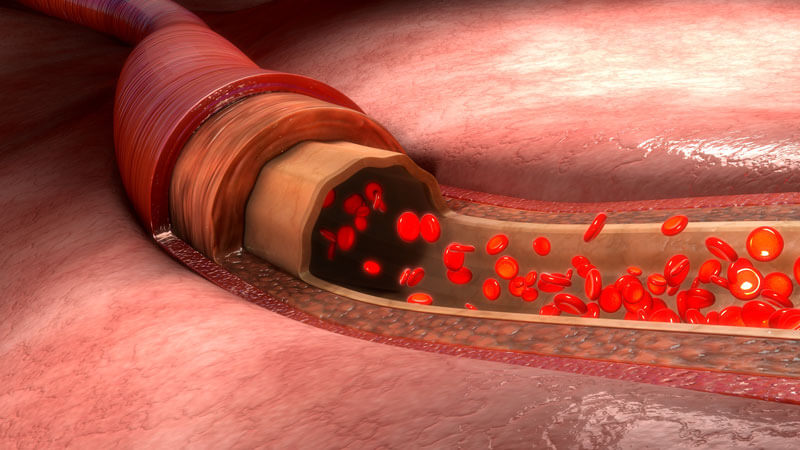
Not only have artery problems been found more often in people who sleep less but vein issues arise as well. In a recent study, scientists saw a decrease in three major miRNAs.
RNAs are vital for the cardiovascular process. When we have fewer of these essential micro RNAs, our veins become inflamed much easier. Inflammation of the veins leads to blood clotting, stroke, and heart attack.
Varicose Veins and Sleep Problems

About six quarts of blood circulate three times every minute throughout your body. This blood carries essential oxygen and nutrients to every cell. When blood flow changes due to varicose veins, more than appearance is at stake.
Varicose veins can cause restless leg syndrome. This may interrupt your sleep-wake cycle, sometimes to a worrisome degree.
Restless leg syndrome just about always occurs when you are laying down or sitting. This specific issue is defined as the irresistible urge to move your legs.
When you are trying to get some sleep, the only way to stop the uncomfortable feeling is to get up and walk around. However, this only removes the issue for a short period of time.
People with RLS report fewer hours of sleep than those without. Typically, they get less than 5 hours of sleep each night.
How Much Sleep Do We Need?

By now you’ve probably heard it a hundred times, but you can never hear it enough. When it comes to sleep, children should have 9-10 hours while adults should have 7-8 hours of uninterrupted rest.
During this time, you should remove anything that may interfere with sleep. Why we need this amount of rest is currently unknown, but we do know it’s vital for staying healthy and happy.
If you have been feeling lucky because you sleep less than the recommended amount but still feel fine – beware! You may be wrong about not needing the same amount of rest as everyone else.
Researchers believe while some people may not feel tired with less rest, the lack of sleep catches up to individuals as they get older.
Fix Your Sleeping Habits
When your sleep schedule gets messed up, it can be hard to get back into a good routine. Here are some tips to getting that much-needed rest:
- If you’re feeling fatigued during the day, start small. Moving your bedtime up 10-15 minutes is a good way to get used to going to bed early.
- Everyone loves a good nap, but your body doesn’t like it as much as you may think. When it comes to naps, you should only be sleeping for 20-30 minutes before 3 pm; never after.
- Caffeine is the enemy to sleep. Try avoiding anything caffeinated in the late afternoon.
- Exerting energy is a sure-fire way of going to sleep early. Make plans to go to the gym for a good run or lift.
NJVVC Can Help You

If your vein problems are affecting your sleep, we have solutions. Our specialists offer the world’s most advanced methods in medical diagnostic technologies.
We can recommend a specialized and precise treatment plan for your unique situation. Our services will relieve your worrisome symptoms and improve your health and appearance.
Please contact us with your questions and concerns or to schedule an appointment. We look forward to helping you!