What You Need to Know About Venous Ulcers
A product of venous insufficiency, venous ulcers are a painful and stressful health issue. Managing this condition means making lifestyle changes. But, how do you know if you have a venous ulcer to begin with? And, are there ways to prevent them?
Here we discuss everything you need to know about venous ulcers: what they are, the risks associated with them, and how to prevent and treat them.
What is a Venous Ulcer?

Venous ulcers or leg ulcers are open sores on your legs caused by poor blood circulation in the veins of the leg. They heal very slowly and can lead to further complications if not adequately treated.
What Causes Venous Ulcers?

Venous ulcers occur as a result of your leg veins not being able to keep blood flowing back to the heart. This leads to blood pooling in the lower legs, especially the bony areas, usually the ankles. Since blood is not flowing properly, the legs swell, exacting pressure on the skin. This results in an open sore otherwise known as an ulcer.
What does a leg ulcer look like?

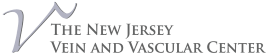
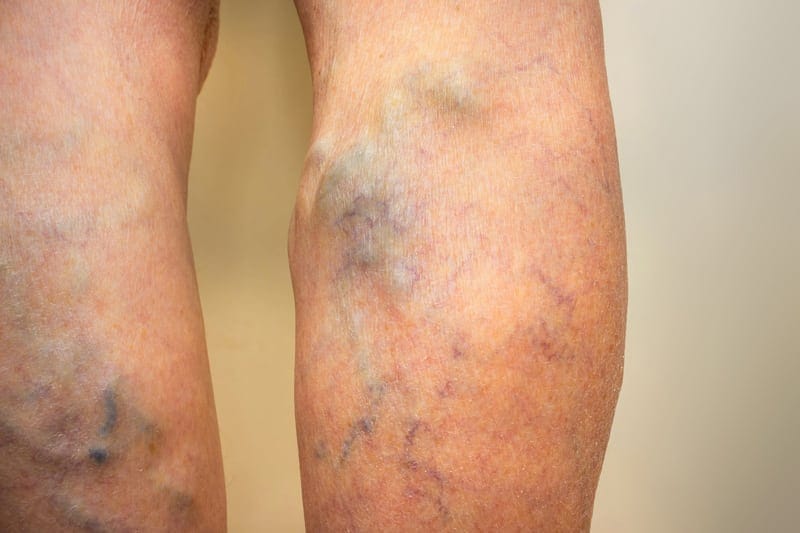
Leg ulcers begin to form when blood pooling in the lower legs goes untreated. The very next sign is stasis dermatitis. Stasis dermatitis is itchy, thin and hardened skin that may have undergone a color change to red, blue, or purple.
You will also notice heaviness, pain, or cramping in your legs. Signs that this condition has advanced into a leg ulcer are:
- A sore with a red base. It may usually be covered by yellow tissue
- Uneven sore borders
- Shiny, tight, warm, and discolored skin surrounding the sore
- Leg pain
For people who think they’re at risk for venous ulcers, you should develop a prevention plan. Ulcers are a very stubborn condition to treat once fully formed. Typically, it takes 3-4 months for your legs to fully heal from a venous ulcer.
Venous Ulcer Prevention
To prevent venous ulcers, you will need to embrace lifestyle changes that promote a healthy flow of blood for the veins in your legs. Preventative methods include:
- Avoiding smoking
- Getting regular exercise
- Staying at a healthy weight – if you are overweight you may want to develop an exercise program
- Not staying in the same position for hours – take breaks to move around
- Moderate your salt intake
- If you have high blood pressure or diabetes, keep it in check
- Wear compression stockings, which can help increase pressure in your leg veins, keep swelling at a minimum, and prevent venous ulcers
Risks Associated with Ulcers
If not properly treated, venous ulcers can lead to severe complications such as:
Skin Infections
The sore may become infected if treatment is ignored. The symptoms of infection include odor, pus, serious pain, and fever.
Bone Infections
When a wound is open too long, bone infections may occur from invading bacteria. Signs of bone infection include fever, muscle spasms, and deep pain in your legs.
Skin Cancer
If your ulcer becomes infected and you continue to ignore it, a malignant tumor may form. Sometimes even with treatment, this may still occur. It is always important to seek medical attention at the first signs of an ulcer.
Management/Treatment

Venous ulcers are not a condition that will go away over time. Without help from a professional, they can escalate to severely painful or even life-threatening conditions.
That’s why this specific type of ulcer requires a lot of care from the patient and treatment from a professional. Treatment of venous ulcers includes:
- Compression stockings, to increase blood circulation in your veins, improving your body’s capacity to heal the ulcer.
- Elevating your legs for 30 minutes 3 to 4 times a day to improve circulation
- Antibiotics to clear the infection
- Surgery to improve circulation. This will help the sore to heal and prevent future blood pooling, as well as the development of future ulcers.
Are you experiencing pain in your legs? Have you noticed any symptoms of venous ulcers? The New Jersey Vein and Vascular Center offers top of the line, personalized vein diagnosis and treatment. We will do our best in expediting your length of treatment to limit your pain and downtime. Contact us today for the highest standard of care.