Can Varicose Veins Cause Hypertension?
For some of us, it seems that the mere thought of varicose veins is enough to cause high blood pressure. But can varicose veins cause hypertension?
High Blood Pressure and Varicose Veins
While there is clear evidence that hypertension can lead to the development of varicose veins, the jury is still out if the reverse is true. The medical community is currently working hard to research the links between high blood pressure and varicose veins.
Right now, there is one thing that they do know for sure. That is, varicose veins can lead to a condition known as venous hypertension.
Venous Hypertension
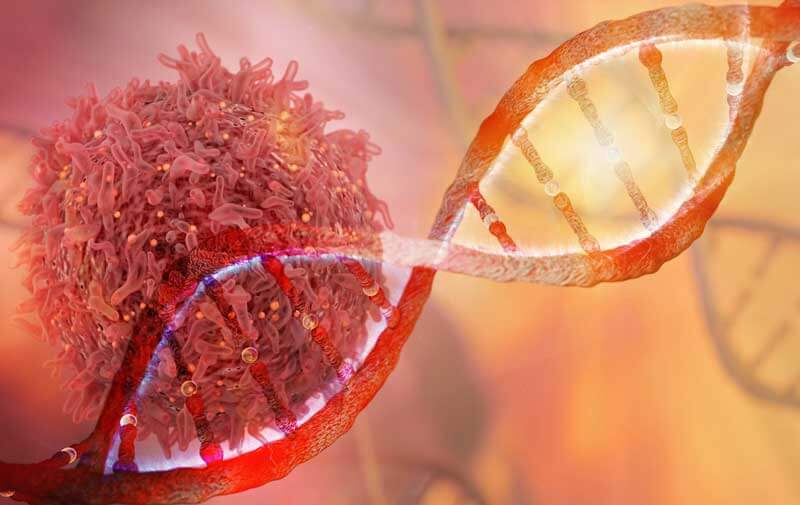
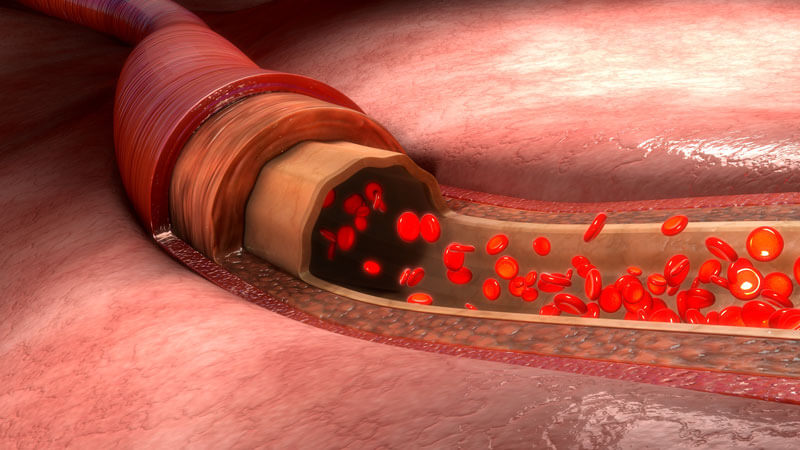
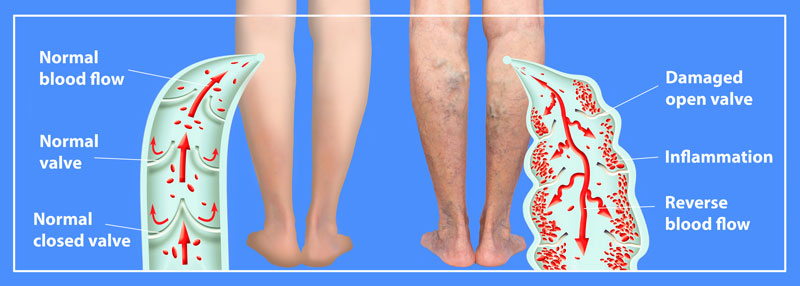
Venous hypertension results when the valves in the veins of the legs are damaged. Damage allows a backflow of blood that begins to pool in the lower legs. As pooling continues, additional strain is put on the heart because greater pressure is needed to transport the pooled blood back to the heart.
Varicose Veins and Your Health

This is a two-way street. Varicose veins may cause venous hypertension and venous hypertension can cause varicose veins. Varicose veins can also lead to a slew of other problems. Ankle flare, edema (swelling), varicose eczema, lipodermatosclerosis, and haemosiderin stainings are all possible issues.
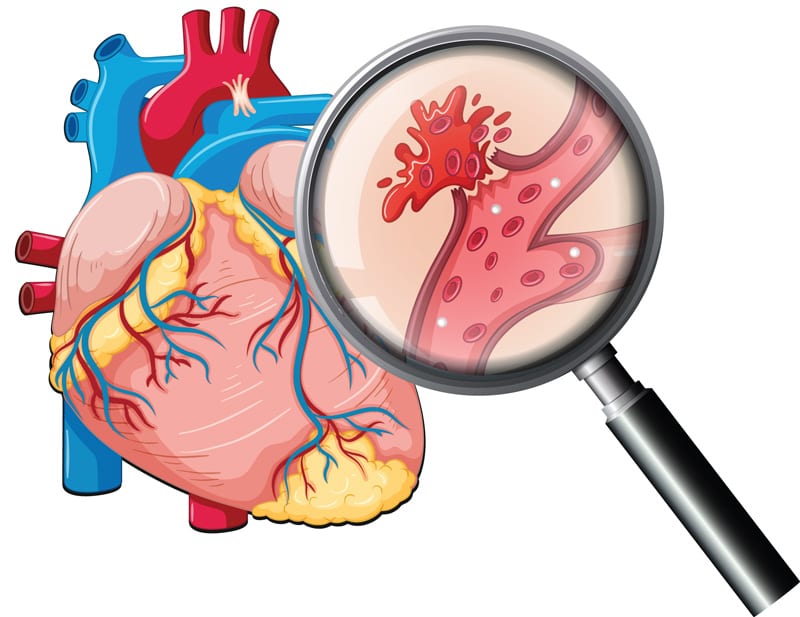
This can be particularly dangerous if you already have any other heart condition. More than one issue can build off each other and develop into heart attacks, strokes, and blood clots. That’s just one reason why varicose veins aren’t just a cosmetic issue, but an actual medical condition.
Varicose veins can also contribute to orthostatic hypotension. This is a marked drop in blood pressure that occurs when going from lying down to standing up.
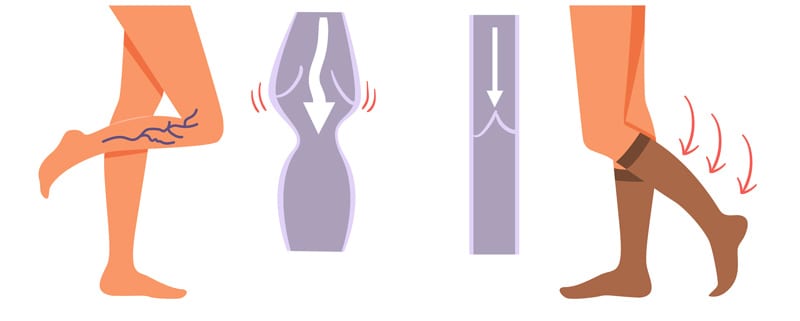
If you’re sick of the heaviness, the aching, and swelling, seek treatment. When you’re done with the pain, itching, burning, and cramps, you can say goodbye to the suffering. There are several treatment options available that will not only improve your venous health, but simultaneously improve the appearance of your legs.
Contact our office to schedule a free consultation. Our staff will listen to your needs. We want to help you find a solution to your painful or unsightly venous conditions.