Mar 18, 2018 | Vein Conditions
One of the many ways pregnancy can affect a woman’s body is through the appearance of varicose veins and spider veins. Although not all women develop them during pregnancy, they are more common after multiple pregnancies and in women with a family history of them. While pregnancy is a beautiful time in a woman’s life, it is also very challenging. Supporting a baby stresses the body and brings about some obvious and uncomfortable changes that leave many women wondering: When pregnancy veins won’t go away, what can be done?
If you develop varicose
veins during pregnancy, you shouldn’t worry immediately. It’s very common. It would still be wise to let your doctor know about them.
If you didn’t have spider or varicose veins before pregnancy, your chances are pretty good that they’ll improve and possibly heal on their own. Spider veins are usually temporary and improve a few months after you give birth. If you did not have varicose veins before giving birth, they will likely shrink or disappear in a few months as well. Although, they’re less likely to go away after
multiple pregnancies.
What Can You Do in the Meantime?
- Get rid of those extra pounds you gained during pregnancy.
- Eat a healthy diet.
- Get regular exercise.
- Don’t cross your legs.
- Don’t stand for extended periods.
- Wear compression socks.
- Be patient.
If three or four months have passed since giving birth, and you still have veins that bother you it’s probably time to seek treatment. Fortunately, there are safe and effective treatments available today that are far less invasive than older approaches.
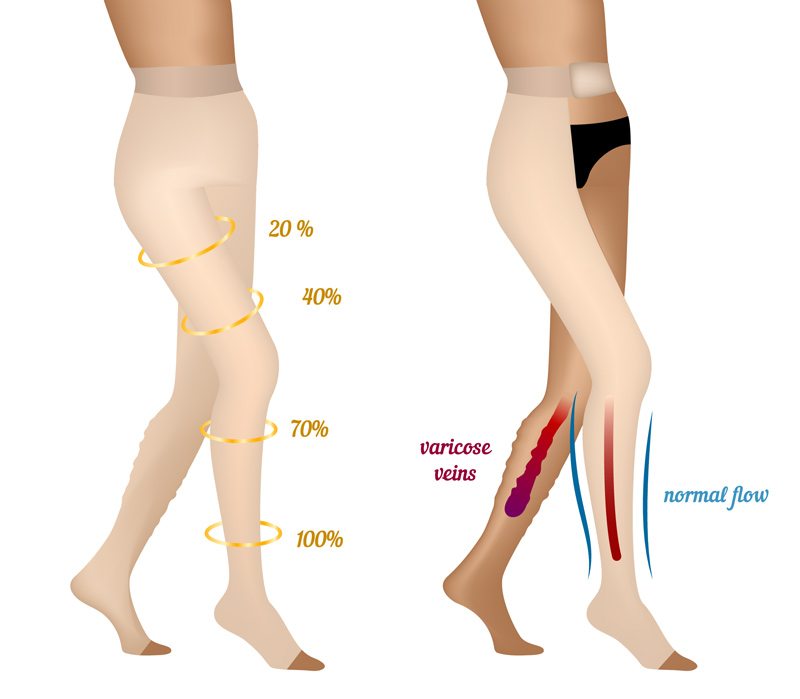
Compression Therapy
It’s often recommended that women wear compression stockings to improve the circulation in their legs, either to prevent varicose veins during pregnancy or to deal with the symptoms. Compression therapy can be very helpful, but it should be overseen by a vein specialist. The level of compression needs to be correctly evaluated.
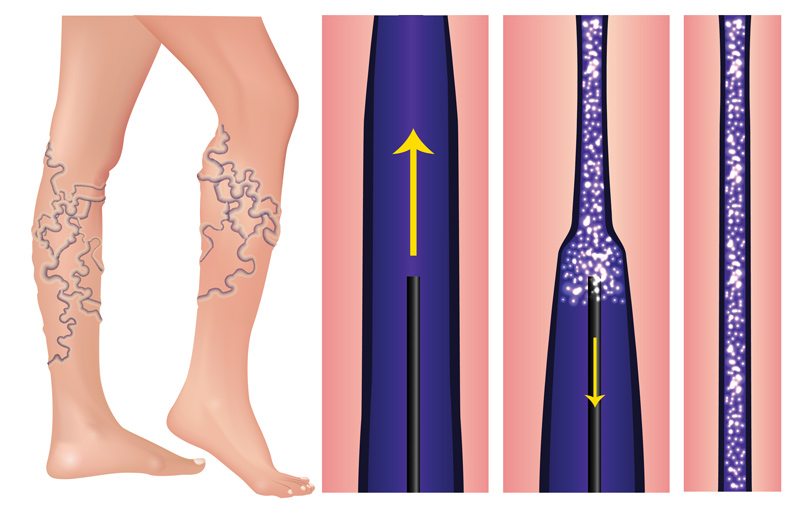
Sclerotherapy
Sclerotherapy is a minimally invasive procedure that only takes 15 to 60 minutes and requires no downtime. A solution is injected into the problem vein, causing it to collapse and be reabsorbed by the body. Larger veins may require multiple treatments.
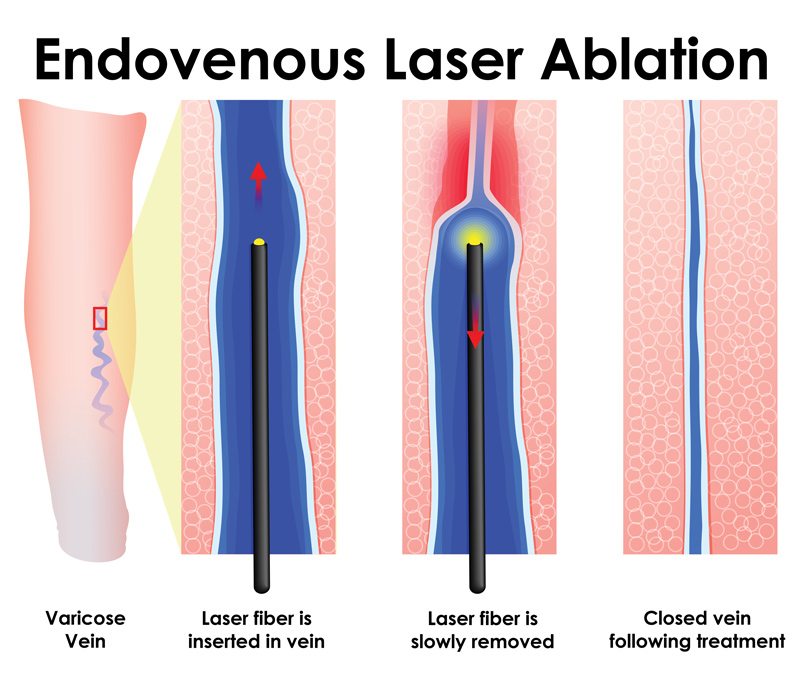
Endovenous Laser Ablation
Endovenous Laser Ablation or EVLT remarkably effective treatment is also known as laser vein ablation. A catheter with a laser tip is inserted into the vein, guided by ultrasound. The laser then seals off the vein, diverting the blood flow. It only requires local anesthesia, is done in about an hour, and doesn’t require multiple sessions. 98% of patients experience immediate relief, and there is no interruption to your daily activities.
If you have concerns or questions about pregnancy veins and treatment options, please
contact us. We offer care and treatment during and after pregnancy.

Jun 29, 2017 | News
A mainly sedentary lifestyle can contribute to the pain and appearance of varicose veins. One of the best ways to improve them is to participate in an exercise program that improves circulation without putting too much stress on your legs and helps with maintaining a healthy weight. Sports and exercising prevent varicose veins so get up and start moving.

Do get out and walk! Walking is probably one of the most important and recommended exercise for varicose vein sufferers, as it is fairly gentle on your legs while promoting circulation. So instead of just grabbing the mail, walk around the block and get your body moving!

Don’t jog or run on hard surfaces. The literal “pounding the pavement” can stress the legs, causing swelling of varicose veins. Instead, try a gentle jog on an even, softer surface such as grass.

Do get in the water! Swimming is a great low-impact exercise that can further develop your calf muscles and aid in improving circulation. This exercise can be done at any level and is great for summer fun.

Don’t participate in high-impact exercise. Heavy weightlifting, while a great workout, can be dangerous for a varicose vein sufferer, as it can put too much strain on the veins of your legs. Using lighter weights with fewer repetitions may be an option if weightlifting is something you love to do. Other such exercises include squats, lunges, and even yoga. Any exercise that increases abdominal pressure can increase leg vein pressure, leading to pain and swelling of varicose veins.

Do get out and bike! Cycling, like walking and swimming, is an ideal low-impact activity that improves circulation while building and strengthening leg muscles. Take a family bike ride in your neighborhood or bring your bike to the park to see more wildlife.

Don’t participate in contact sports. In sports such as football, rugby, and even tennis and skiing. The high probability of injury and sudden, quick movement can be counterproductive to leg vein health.

Starting with walking, cycling, or swimming for 30 minutes a day is a great way to alleviate the pain and appearance of varicose veins.
For more information about your vascular health, contact NJVVC today!