Do you have clusters of red, blue, or purple veins on your ankles or feet? Are these veins thin and close to the surface of the skin? If so, it sounds like you have spider veins. Many people come to...


Do you have clusters of red, blue, or purple veins on your ankles or feet? Are these veins thin and close to the surface of the skin? If so, it sounds like you have spider veins. Many people come to...

This blog covers the first signs of leg ulcers and both medical and at-home treatments. We’ll discuss why it’s important to examine the underlying causes and how to reduce and prevent their frequency. An ulcer is an open sore on...

This blog covers the basics of venous insufficiency a precursor for chronic vein insufficiency( CVI). It also goes into detail about the symptoms, causes and common treatments of CVI. Over 40% of people in the United States have chronic venous...

Menopause dramatically reduces the amount of estrogen and progesterone produced in the ovaries. Because of that, women over 50 are at a higher risk of developing varicose veins. Estrogen and progesterone contribute significantly to the health of women’s capillaries and...
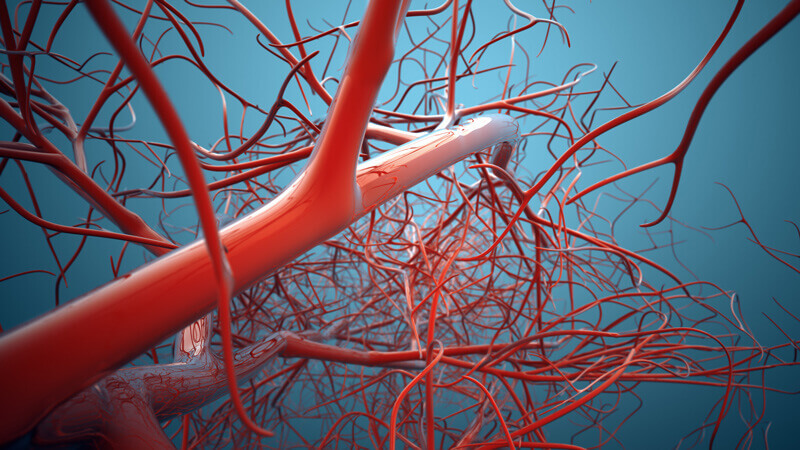
Good vein health can’t be achieved overnight. It takes eating the rights foods, exercise, and putting aside some bad habits. An estimated 40 million Americans are affected by varicose veins, which is just one type of vein complication. About half...

Diabetes affects over 30 million Americans, according to the most recent data provided by the CDC. People most often attribute diabetes to blood-glucose levels, insulin, and even diabetic shock. But diabetes negatively affects the body in other ways. One area...