Dec 21, 2021 | Spider Veins, Vein Conditions, Vein Treatments
Do you have clusters of red, blue, or purple veins on your ankles or feet? Are these veins thin and close to the surface of the skin? If so, it sounds like you have spider veins. Many people come to our vein center asking about the spider veins on their ankles and how to treat them.
What Are Spider Veins?
Spider veins develop when blood gathers in the veins that exist near your skin’s surface. These veins have stopped working efficiently because they are weak or damaged. Blood backs up and pools, causing the veins to become visible.
Why Are Spider Veins Commonly Found on Ankles and Feet?
Ankles and feet are prone to developing spider veins. Slower blood circulation and increased pressure on veins causes feet to swell. This encourages the formation of spider veins.
You also find spider veins on the thighs, calves, and face.

What Factors Influence the Development of Spider Veins?
Heredity plays a major role in the development of spider veins. In fact, studies show that up to 90 percent of people who have spider veins have a family history of them.
Other factors can include:
• Sitting or standing for long periods of time
• Obesity
• Trauma
• Sunlight exposure
• Pregnancy

What Do Spider Veins on Ankles Look Like?
Spider veins have a specific look. They seem to gather and branch out from a central location. Each vein is usually less than 1mm in diameter.
This common grouping of veins often resembles a branch, a spider, or a spiderweb. Now you know where the name “spider veins” comes from!
When blue and/or red spider veins are on the inside of the ankle or foot and form a crown-like pattern, it is called corona phlebectasia. This is associated with advanced vein problems. People with corona phlebectasia should visit a vein doctor for a complete diagnosis and treatment plan.
Symptoms of Spider Veins
Spider veins on the ankles, although unsightly, usually don’t indicate a serious health problem.
Sometimes they are itchy or painful. But most often, spider veins are mainly annoying from a cosmetic standpoint. Understandably, people want unattractive spider veins treated.
In rare cases, spider veins contribute to the formation of large skin sores, or ulcers. This problem is most likely to occur near spider veins on the ankles and requires immediate treatment.
Treatment for Spider Veins on Ankles
Excellent treatment exists for unattractive spider veins on feet and ankles.
You can try some simple things at home to ease minor discomfort and prevent additional spider veins from forming.
Unfortunately, untreated spider veins will worsen over time.
To eliminate existing spider veins, visit our office for safe and effective treatment.

Ways to Prevent Spider Veins on Your Ankles
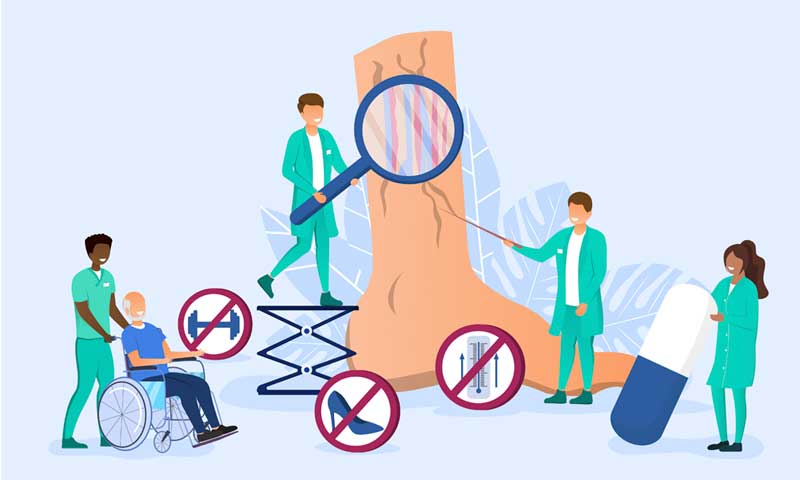
When sitting, keep your feet elevated above your heart. This will improve your circulation and can even reduce the size of spider veins in your ankles and feet. Use a recliner or put pillows under your feet in bed.
Wear compression socks. Compression socks will improve your blood circulation and reduce pressure on leg and foot veins. Your feet will not swell, reducing the development of more spider veins.
Try not to stand for a long period of time. And try to stand on your tiptoes at workable intervals. This will improve leg muscles and blood circulation in spider veins.
Exercise more. Increase your physical activity to reduce vein discomfort. Regular-paced walking will improve your spider vein health.
Learn useful massages for your ankles and feet. Our doctor can discuss what type of massage will work best in your situation.
Visit Our Office for a Spider Vein Evaluation
Patients come to our office for accurate diagnosis and state-of-the-art treatment of spider veins and other vein issues.
At NJVVC, we know the importance of thoroughly understanding your vein health. We perform comprehensive vein evaluations so we can successfully treat your spider vein problems.
Sclerotherapy Treatment for Spider Veins
Before our doctor treats your spider veins, he will make sure they aren’t associated with varicose veins. If our doctor finds this connection, he will first treat your varicose veins; this will keep the spider veins from reappearing after treatment.
Spider veins in themselves may not be a serious problem, but varicose veins often need treatment.
Visual Sclerotherapy is extremely effective in the treatment of spider veins. It involves injection of a solution into the spider vein. The solution causes the vein to collapse.
This treatment requires no anesthesia.
The sclerosing agent that we use at NJVVC is safe and comfortable for the patient. Your treated spider veins will collapse and disappear three to six weeks after your procedure.
If you have spider veins or other vein issues, contact us for an appointment. We offer expert diagnosis and treatment.

Aug 21, 2021 | Leg Care, Skin Conditions, Vein Conditions, Venous Insufficiency
This blog covers the first signs of leg ulcers and both medical and at-home treatments. We’ll discuss why it’s important to examine the underlying causes and how to reduce and prevent their frequency.
An ulcer is an open sore on your skin. Ulcers can affect any area of your skin, but often, they occur on the legs.
Leg ulcers can be very painful and often take as long as three to four months to heal, with appropriate treatment.
The most common cause of leg ulcers is poor blood circulation in your veins. This can lead to several other issues including chronic vein insufficiency. Early detection is key in preventing irreparable damage.
Anatomy of Leg Ulcers
A leg ulcer is a chronic sore that develops between your knee and your ankle. They typically appear on your inner leg near your ankle and may take several weeks if not months to heal.
They present as large, red, swollen, fluid-seeping sores with irregular edges that are resistant to healing.

Generally, ulcers are characterized by how they look, their location, the surrounding skin.
Some causes of leg ulcers include:
• Lymphedema
• Venous Disease
• Peripheral Arterial Disease
• History of Leg Ulcers
• Deep Vein Thrombosis (DVT)
• Undergoing Surgery or Injuring an Infected Leg

Signs and Symptoms
Most symptoms of vein disorders are transitory and can be effectively treated. However, venous leg ulcers are much more challenging and severe.
The heightened risk of an open sore getting infected is what distinguishes it from other diseases. If left untreated, a venous leg ulcer can have a negative impact on your health.
Signs of leg ulcers may include aching and tightness in your calves. Throbbing or a heavy feeling in your legs may also signify their coming appearance.
Once an ulcer develops, you may see discolored splotches around the edges due to pooled and trapped blood.
Some leg ulcers will only affect the skin, however, there are times when the sore may descend deeper into your muscle, your tendon, fat layer, or bone.
Risk Factors
Women are at a higher risk of having Venous leg ulcers. Women affected tend to be in their forties, while the men affected tend to be in their seventies. Other possible causes for venous leg ulcers include:
• Cancer
• Obesity
• Smoking
• Immobility
• Pregnancy
• Varicose Veins
• Heredity/Genetics
• Incompetent Valves
• Swelling of a Superficial Vein (phlebitis)
• Muscle Weakness in the Legs, Leg Injury, or Trauma
A majority of ulcers heal within three months. However, some ulcers may take years to heal and about 15% may never completely heal.

Seeking Medical Help
You should contact your doctor if you have a wound that will not heal, or if you think that your wound is infected. Your doctor should inquire about any history of recurring or chronic conditions, like diabetes or hardening of the arteries.
In some cases, additional tests such as an X-ray or CT scan may be needed.
Signs of a wound or leg ulcer infection can include:
• Chills
• Odor
• Fever
• Bleeding
• Increased Pain
• Excess Drainage
• Swelling About the Wound
• Redness, Increased Warmth
• Cloudy or Yellowish Drainage

Diagnosing Leg Ulcers
A physician will perform a Doppler Study to evaluate your veins and arteries. During a Doppler Study, an ultrasound probe is placed on the skin in order to visualize blood flow patterns.
Your doctor may also obtain blood pressure readings at your arms and ankles for comparison if he/she suspects arterial disease.
Treating Leg Ulcers
Some treatment options are non-invasive, while other methods are medically involved. Treatment options are administered based on the severity of your condition.
Medical treatment strives to enhance blood flow to the affected area as well as encourage recovery of the ulcer.
Practicing Prevention
Here are some things that you can do at home to prevent a leg ulcer.
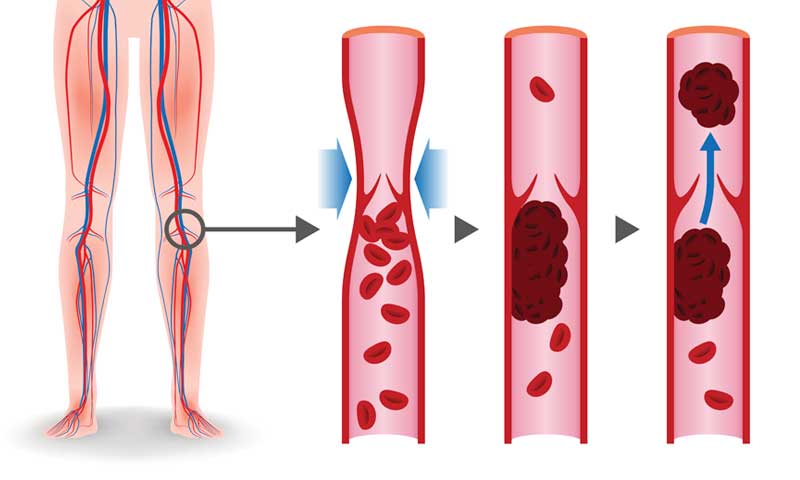
Compression Stockings
Compression stockings assist in reducing strain and edema on the skin due to increased pressure and swelling.
Elevate Your Legs
Elevating your legs will help in circulating blood back to your heart. Also, use a pillow to prop up your feet when sleeping, and elevate your legs above your heart for 30 minutes when you awaken, and repeat up to four times daily.
Maintain Healthy Skin
Keep your lower legs clean and moisturized with a non-drying, alcohol-free moisturizing cream or lotion.

Exercise
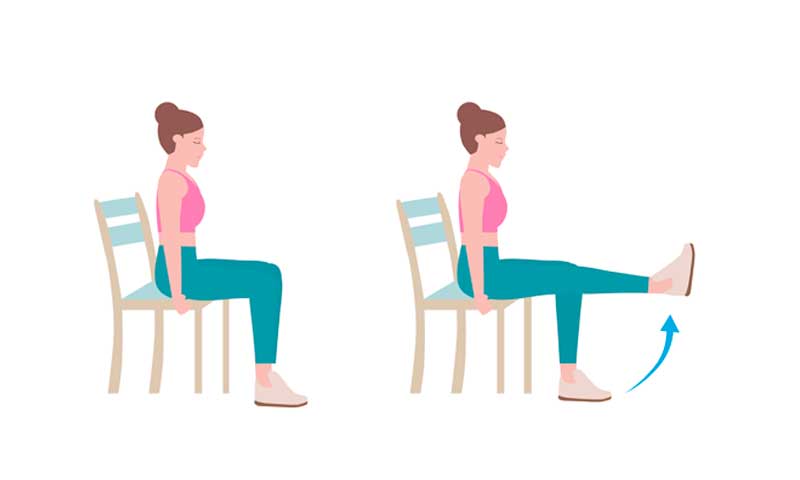
Exercise is known to promote healthy veins and blood flow. Daily exercise is also an awesome way to increase circulation. Foot and ankle exercises can promote good blood flow. So, give it a try.
Point your toes upwards, then point them away from you. Repeat this exercise for a few sets every day. This can be done in a sitting or standing position.
New Jersey Vein and Vascular Center in Morris County is committed to personalized patient care and good vein health.
Our state-of-the-art vein center maintains the highest standards and advances in the field of vein and vascular care. Our goal is to diagnose and treat the underlying causes of your various vein conditions.
For more on our office and services, please contact us today.

Jun 21, 2021 | General Health, Vein Conditions, Venous Insufficiency
This blog covers the basics of venous insufficiency a precursor for chronic vein insufficiency( CVI). It also goes into detail about the symptoms, causes and common treatments of CVI.
Over 40% of people in the United States have chronic venous insufficiency. Early detection is key to preventing damage caused by vein disease.
That’s why we’ve put together a guide on everything there is to know about CVI and how a vein specialist can help remediate symptoms.
What is CVI?
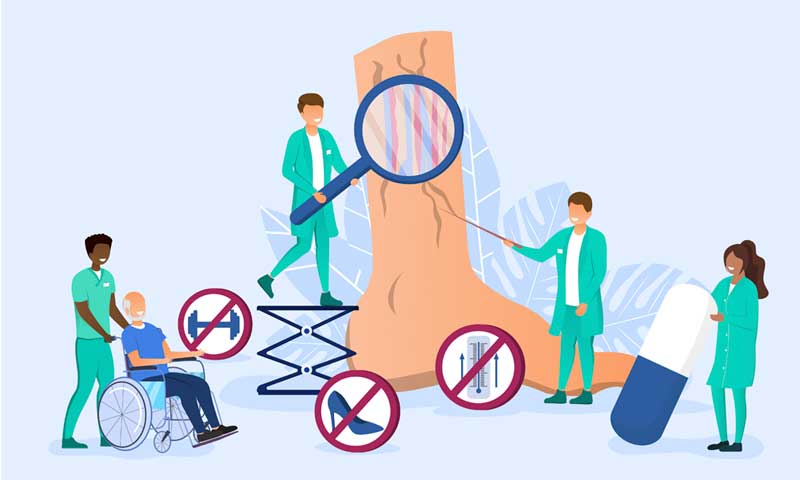
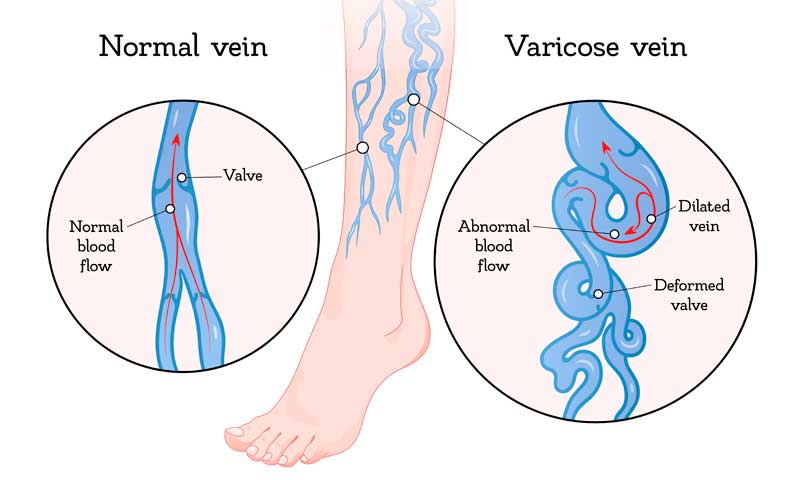
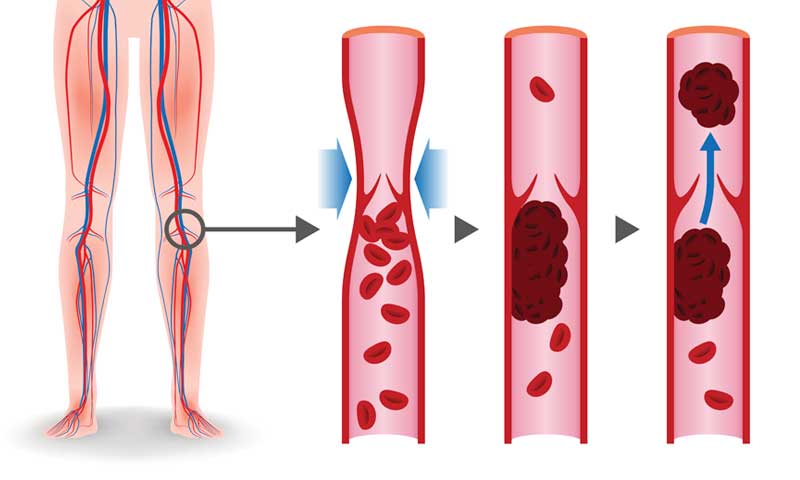
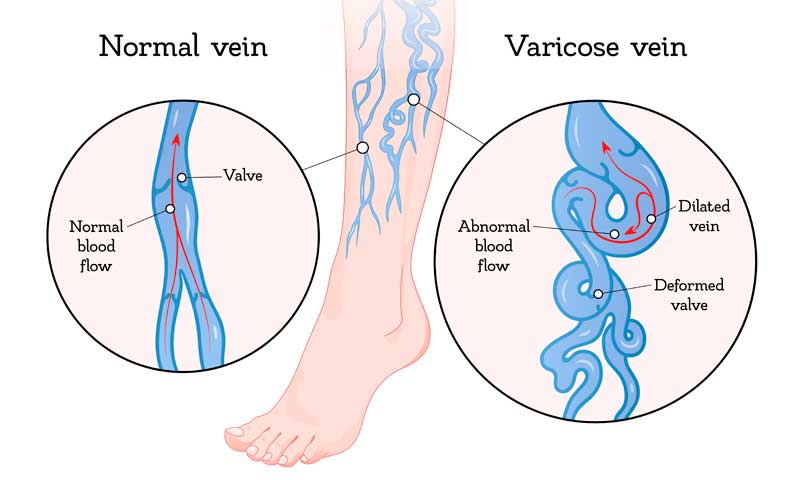
Chronic venous insufficiency or CVI is an acute or persisting form of venous insufficiency. Venous insufficiency is a vein disease that occurs when valves in the leg are not working properly.
When these valves are not functioning, it becomes difficult to return blood to the heart. Blood will then begin to collect and pool. The “pooling” of blood in our veins is called stasis.
What Causes CVI?
First, let’s go back to basic biology with the anatomy of a vein and our circulatory system. Our heart pumps blood through the arteries to our entire body to keep it functioning.
Our veins are responsible for returning blood to the heart. In order to reach the heart, our blood needs to flow upward from our legs.
To do this, our leg muscles contract while walking. This causes our veins to push blood against gravity and towards our heart.
However, something else needs to be in place to keep our blood flowing up, not down. That’s where valves gain their importance.
Each vein in our legs contains one-way valves. These valves are responsible for keeping blood flowing in an upward direction.
When they are not properly functioning, valves no longer have the ability to direct blood. This allows blood to pool and collect which causes CVI.
Valve damage is a common cause of CVI and can occur due to several reasons. It can result from simply aging or from extended sitting and reduced mobility.
Although, the most common cause of CVI is Deep Vein thrombosis (DVT).
CVI vs DVT
DVT occurs when a blood clot forms in one of the veins deep inside your body.
CVI differs from DVT mainly due to its causes. CVI can often occur without a clear-cut reason whereas DVT happens because of immobility.
People often develop blood clots after surgery or traveling for that reason.
Learn more about understanding and preventing DVT.
Symptoms of CVI
Over time, CVI can cause many symptoms and affect our bodies in more ways than one.
CVI can cause severe pain and swelling in your legs, feet, or ankles. It can also cause changes to the skin on your legs that lead to ulcers or open sores.
Venous ulcers are painful and notoriously known to be very difficult to heal. Venous ulcers also have a high tendency to become infected, causing even more trouble for your body.
If you have any symptoms of CVI, it’s better to see a doctor sooner rather than later. Non-invasive treatments become limited if the disease is left untreated.
Here are more common symptoms of CVI:
• Swelling in lower legs or ankles
• Aching in legs
• New varicose veins
• Flaking or itching skin near legs and feet
• Stasis ulcers

Stages of CVI
The severity of CVI depends on how long it’s left untreated. Symptoms of CVI increase as the disease progresses and so do the hidden health risks. Therefore, getting an early diagnosis of CVI can be the difference between having subtle or severe symptoms.
Once showing the common symptoms of venous insufficiency, patients should seek medical advice from their doctor.
For a formal diagnosis, your doctor may use a venous ultrasound to examine the blood circulation in your legs.
When left untreated, CVI can often reach a dangerous stage. Eventually, the pressure and swelling will get too much for our veins to handle.
This can lead to blood vessels in our legs bursting. The overlying skin in this area is then very sensitive and susceptible to cracking.
Treatments
After diagnosis, your doctor may treat CVI and its symptoms using several different methods.
These can include compression stockings or antibiotics, depending on the severity of the case.
The overall goal should be to improve your circulation and decrease venous insufficiency.
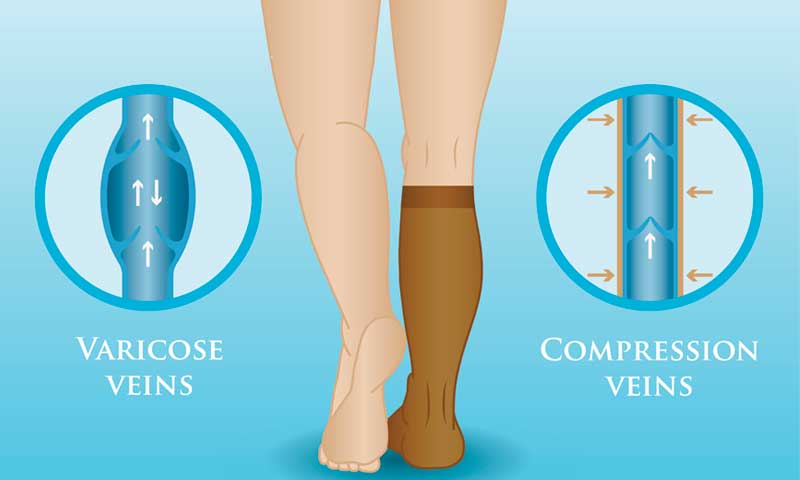
Compression Stockings
Compression stockings are the most common treatment for mild cases of venous insufficiency.
Compression stockings are lightly-fitted support stockings or socks.
Compression therapy aids the body in moving blood up the leg against the pull of gravity. They are used to improve circulation and reduce swelling in the legs.
Compression therapy is also used to aid in healing after various types of vein surgery.
Antibiotics
A doctor may prescribe antibiotics to resolve any skin issues related to CVI. Issues can include deep skin infections caused by ulcers or sores.
Antibiotics will not treat the underlying issues of CVI, but they can still help clear up skin problems that manifest.
Sclerotherapy
Sclerotherapy is the most common spider vein and smaller varicose vein treatment. It involves injecting a solution directly into veins. The solution then causes the veins to collapse and disappear.
Sclerotherapy is one of the easier solutions to vein issues. Treatment time depends on the specific case but can take anywhere from 15 minutes to an hour. Sclerotherapy is minimally invasive and requires only topical anesthesia.
Sclerotherapy is typically used to treat spider veins or varicose veins. However, it can also treat symptoms of CVI. Treated veins usually disappear in three to six weeks. Some larger veins take longer.
Up to 80% of the spider veins treated will disappear with each treatment.
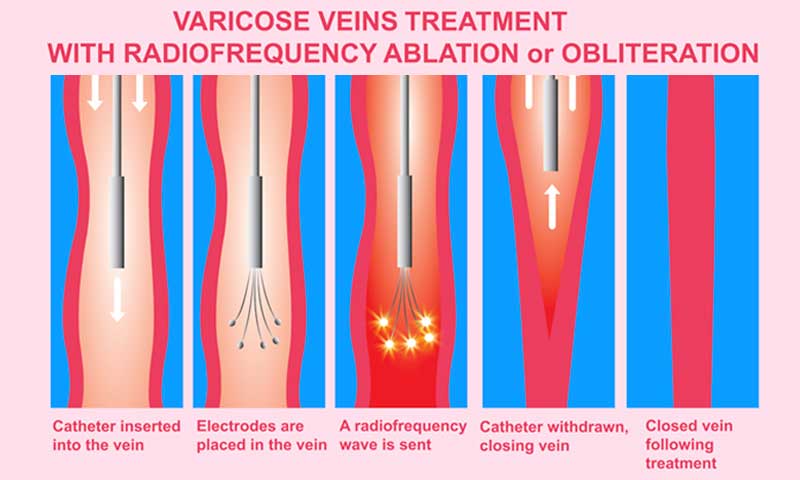
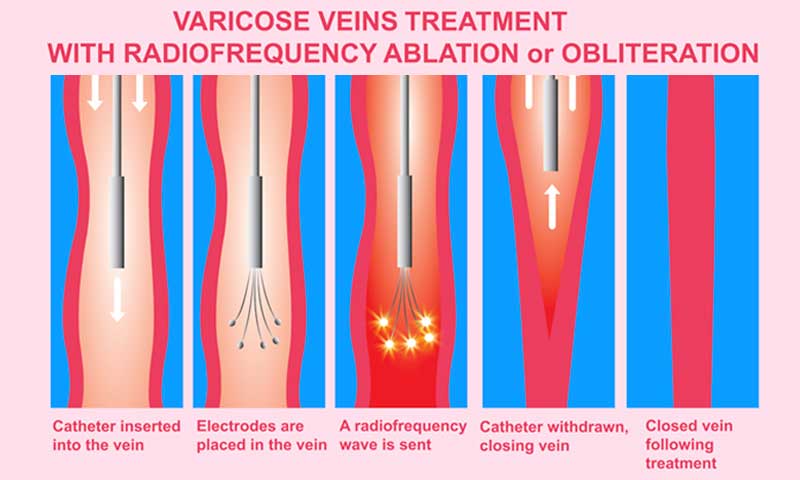
Endovenous Thermal Ablation
Endovenous Laser Treatment (EVLT) is a superior treatment for vein problems. It is also known as laser vein ablation or obliteration.
Unlike conventional surgery, EVLT provides much less risk and is extremely precise.
A catheter with a laser tip is inserted into the vein. Ultrasound imaging helps guide exactly where to position the laser. The laser tip catheter is then activated inside the affected vein to shrink it down and seal it.
This stops the blood flow to that vein and diverts it into others. It increases circulation and relieves existing symptoms of CVI.
This outpatient treatment takes less than an hour and is minimally invasive. Relief of symptoms begins within several days of the procedure.
Ambulatory Phlebectomy
Ambulatory phlebectomy is a minimally invasive outpatient procedure. It involves removing incompetent, superficial, or varicose veins.
This treatment is usually done on larger veins that bulge above the surface of the skin.
CVI can often be debilitating to deal with. But a CVI diagnosis does not mean you’re left without options. There are many treatments available to ease symptoms and vein issues. Finding the right vein specialist is the first step to recovery.
At the New Jersey Vein and Vascular Center, we’re committed to personalized vein care. Our goal is to diagnose and treat the underlying causes of various vein conditions.
For more on our vein services and treatments, please contact us today.

Apr 21, 2021 | General Health, Prevention of Vein Conditions, Vein Care
In this blog we break down the connection between exercise and healthy veins. We’ll cover everything you need to know, including which exercises are best for you.
Exercise promotes a healthy body. It aids in strengthening your immune system, increases weight loss, and even improves mental health. But did you know exercising also promotes healthy veins?
Healthy veins have good blood flow. They provide proper circulation throughout the body.
The best way to promote quality blood flow is to move your muscles with exercise.

What Exactly Do your Veins Do?
Knowing about the anatomy of your veins is a vital part of staying healthy.
Going back to basic biology, blood flows through our bodies using veins and arteries. Your veins are vessels that transport blood to your heart, while your arteries carry blood away from it to your extremities.
Veins carry nutrients and water needed for your body to function. They also carry blood to the heart, where “old” blood receives a fresh supply of oxygen.
Healthy veins are able to keep the body infused with enough oxygenated blood. Unhealthy veins do not function as well and allow blood to pool.
When blood does not flow properly, it causes a backup of blood in veins. This pooling enlarges veins and pushes them near the surface of the skin.
Learn more about varicose veins causes, symptoms, and treatments.
How to Recognize Unhealthy Veins
Varicose veins, or bulging veins, are common in both men and women. In fact, around 23% of the American population has bulging veins.
Varicose veins alone are not life-threatening but can be extremely uncomfortable. Common causes of varicose veins include heredity, lack of activity, and age.
Women who are menopausal can also have an increased risk of varicose veins due to hormonal changes.
Symptoms of vein issues can include leg fatigue, cramps or aches, and swollen feet or ankles. If you have any of these symptoms, it could be an indicator of poor vein health or a vein condition.
The good news is you can manage these symptoms with daily exercise. But always talk to your physician before starting if you have underlying health issues.
How Does Exercising Promote Healthy Veins?
Regular exercise prevents obesity and harmful weight gain. Being overweight puts more stress on veins and valves in our bodies. This forces our veins to work harder to keep blood flowing.
Obesity also weakens the heart muscles and can reduce the flow of oxygenated blood. This all adds up to a poor circulatory system and can lead to more serious health issues.
Exercise promotes healthy veins by stimulating the flow of blood. As mentioned above, good blood flow is necessary for our bodies to perform – so get up and move!

What Kind of Exercises Are Good for Veins?
Exercises that involve your legs are the most effective for vein health. They stretch your muscles to make blood flow upward towards the heart.
Finding simple ways to improve circulation will benefits your whole body, not just your veins.
If you are one of the 23% who suffers from bulging veins, ditch the heavy lifting. You should avoid exercises that put too much pressure on your body and veins. Lifting weights can increase pressure on veins that are already stressed and bulging.
Instead, you should aim for moderate exercises that use the calf and thigh muscles. These are great for enhancing blood flow to and from the lower and upper half of your body.
Walking, bicycling, and swimming are the best physical activities to reduce vein pressure.
Here are a few other easy-to-do, vein-promoting exercises to try at home:

Butt-Kick
While standing in place, raise your heel to reach your buttocks. Try “kicking” your butt every few seconds while alternating between legs. Do this for 30 seconds to a minute a few times a day.
This exercise strengthens thigh and buttock muscles that support blood flow.
To increase the impact of this exercise, jog in place while completing repetitions.
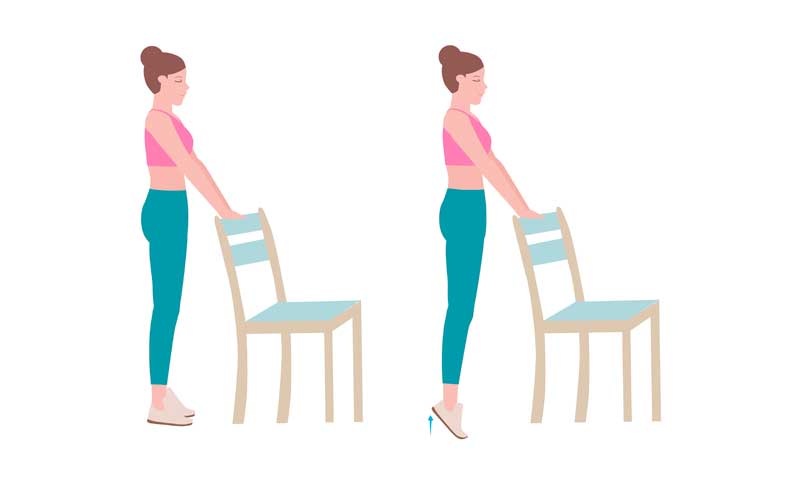
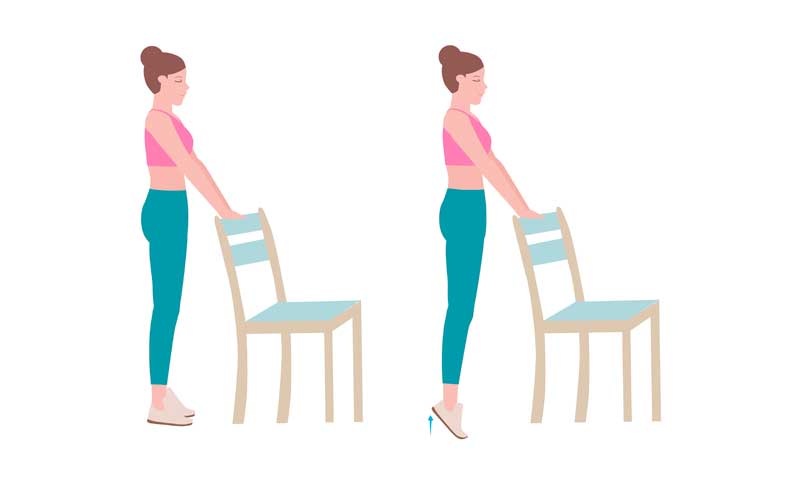
Calf Stretch
Stand behind a kitchen table chair and grab onto the back to keep steady. Lift yourself using only your toes.
Hold that position for five seconds, and then lower yourself down. Try doing 15 to 20 raises in a row before taking a break.
Toe lifts
Start by sitting in a chair or on the floor, with your feet flat on the ground. Lift your toes up, just your toes not your whole foot.
As you’re lifting your toes, try to get them all to the same height if possible. Hold this position for 5 seconds, then lower your toes.
Repeat 10 times on each foot or do both feet together.
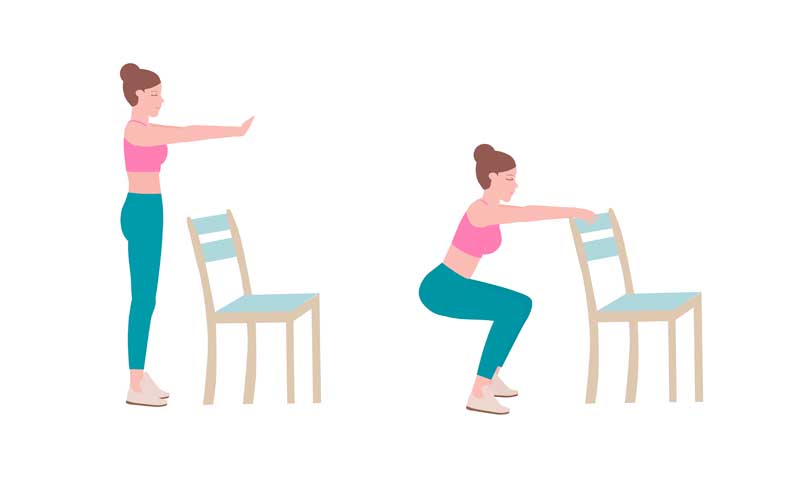
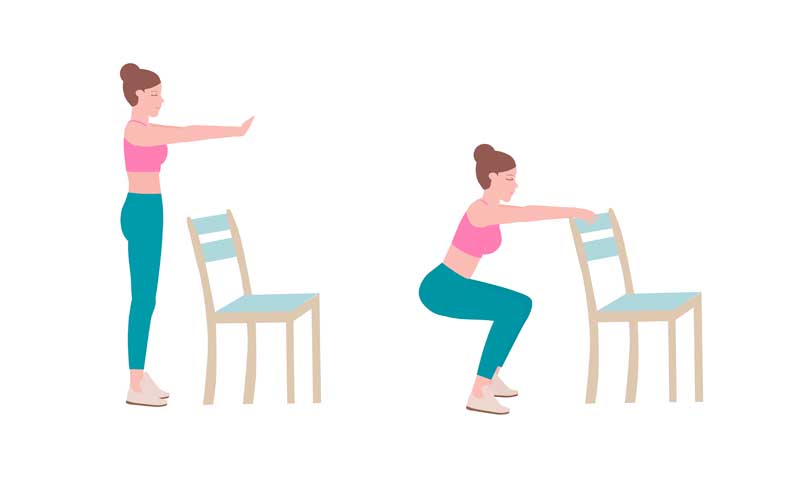
Squats
From a standing position, lower your body like you are going to sit down. Once you have reached a seated position, use your leg muscles to resume standing.
If you have balance issues, you can do squats against a wall for added support.
Lunges
Start in a standing position, with legs shoulder-width apart. Step forward with one foot until your leg reaches a 90-degree angle.
Then lift your front lunging leg to return to the starting position.
Repeat in this position for more reps, or change legs between each rep.
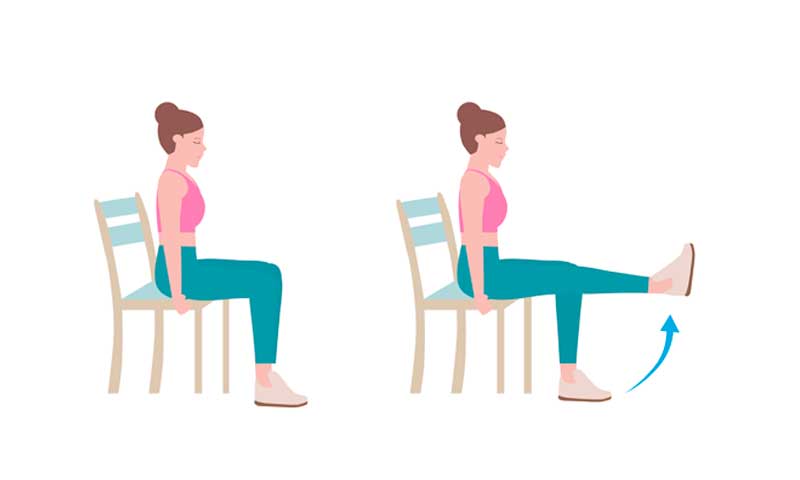
Leg lifts
Leg lifts allow blood to move from your feet towards your hips.
Sit or lie on your back with your legs straight out. If you prefer to stay off the floor, sit in a chair with your feet flat. Slowly lift one leg and hold it in the air for at least five seconds before lowering back down. Repeat the exercise with your other leg.
Bicycle legs
Lie on your back and raise your feet in the air, bending your legs at your knees. Pedal your legs as if you were riding a bicycle.
You can also do this exercise one leg at a time, alternating legs between sets.

Yoga Stretches
Yoga benefits the cardiovascular system. It is the perfect low-impact workout for our bodies. It doesn’t put pressure on our veins or joints which makes it ideal for all.
Stretches like downward-facing dog, chair pose, and warrior pose are great for veins.
NJVVC Vein Services
Your health and well-being rely on the health of your veins and arteries. At New Jersey Vein and Vascular Center, we commit ourselves to personalized patient care and good vein health. Our vein center maintains the highest standards and advances in the field of vein and vascular care.
Schedule a consultation appointment with a certified vein doctor. Learn more about varicose vein removal in NJ with our experts. Contact us today!

Mar 21, 2021 | General Health, Leg Care, Prevention of Vein Conditions, Skincare
We all know the drill. Once the winter chill sneaks in, it’s easy to lack moisture and mobility in our lives. Our skin gets drier and our muscles get tighter. This means our legs need extra attention and care during the winter months.
You may have noticed your skin gets dry when the cold weather begins. But winter brings more than dry skin. If you’ve also noticed leg cramps and soreness, you’re not alone. These symptoms are common in many people and can be exacerbated by the cold.
But there’s good news. You can combat both dry skin and leg cramps this winter season. Read over these helpful tips your legs will love.
How to Combat Dry Skin:
Reduce Shower Time
What’s not to love about a long, hot shower when it’s freezing out? But did you know those hot showers could be drying out your skin even more?
Reduce the amount of time you spend in a hot shower or bath by half. Try to keep your shower time to 10-15 minutes or less.
Use Gentle Cleansers
You may have heard the term pH balance in the skincare world before. But if you haven’t, let’s go back to the basics. pH stands for potential hydrogen, which is a measure of the element’s activity in a substance.
The pH scale ranges from 1 to 14. A pH level of seven is neutral and anything lower is acidic. Anything higher than 7.0 is considered in the alkaline range. Skin tends to be naturally acidic and depending on the area of skin tested, it usually averages between 4.7 and 5.0.
An ideal skin pH is between 4.7 and 6.0, which is slightly acidic. Many soaps or body washes score over eight on the pH scale. The use of certain products disrupts the skin’s ability to maintain a healthy pH level. This could be a major reason why the skin on your legs is dry, flaky, itchy, and inflamed.
Drink Water
Staying hydrated is key for your skin to retain moisture. Try to drink more water. It’s easy to drink plenty of water in warmer weather. Nothing is more refreshing on a hot day than a tall glass of ice water
But when it’s cold, we tend to reach for hot lattes, which dehydrate our body. Even more so if you’re not drinking enough water to counteract the caffeine.
Exfoliate
One of the most important tips for having smooth, healthy skin is exfoliation. Exfoliation is the removal of dead skin cells from the surface of our skin.
Did you know our skin naturally sheds dead skin every 30 days? But sometimes, dead skin cells don’t shed completely. This leaves the skin looking dry and flaky.
The key to exfoliating in the winter is knowing how often to do it. Meaning, don’t exfoliate more than once a week as it can be too harsh for your skin.

To exfoliate the legs, try “dry brushing”. This is exactly what it sounds like: brushing your skin with a dry brush. Brushing the skin while it’s dry will loosen dead skin so it will wash off easily in the shower.
Eat Fatty Acids
Eat more foods containing essential fatty acids (omega-3 and omega-6) such as lean meat, eggs, walnuts, and salmon. The body cannot make these fatty acids on its own. But they are essential for proper skin hydration and health.
Quit Smoking
Nicotine is a known blood vessel constrictor that can reduce oxygen levels in the body. Insufficient oxygen may lead to pale, itchy dry skin that worsens in winter.

Smoking also increases the risk of varicose veins, leg soreness, and leg ulcers. If you smoke, ask your doctor about medications or programs available to help you stop.
Moisturize
Hydration is key for many aspects of our bodies. Our skin needs to retain moisture to function properly. Basic moisturizers will do the trick on the surface of the skin. But oils work to lock-in moisture deeper into the skin.

Skin oils, like baby oil, also act as a protective barrier between dry air and our skin. Try rubbing a few drops of baby oil on your legs after a shower.
Winter Leg Cramps
Now that we have our leg skin ready to combat the cold, let’s move on to our muscles.
Why Do Muscles Cramp More in Winter?
Muscles contract when they get cold as a way of preserving energy. This means you must exert more force to move your muscles in the cold.

Not using our contracted muscles increases stiffness, spasms, and cramps. Add slight dehydration during the winter, and you’ve got achy, tired legs.
For Muscle Pain Relief
Epsom Salt Soaks
Soak your legs in Epsom salt to soothe your muscles. Epsom salt is a magnesium sulfate compound used as a healing agent and pain reliever. Magnesium works well for relaxing constricted muscles and heal minor inflammation.

If you don’t feel like getting in the tub, just give your feet some love. Make a foot soak by filling your bathtub or a basin with water that covers your feet. Then add a 1/2 cup of Epsom salt and soak your feet for about 30 minutes. You’ll provide your feet with some relief and your legs will thank you.
Heating Pads
Place a heating pad or a moist cloth warmed in a microwave on achy areas of your legs. Note that moist heat is always better, as the hot moisture gets absorbed into the muscles.
Hydration is one of the most important things needed for our muscles. The Institute of Medicine (IOM) recommends drinking 10-16 cups of water a day.
If you have a bad habit of forgetting to drink water, don’t worry. Look for water bottles that light up or flash when it’s time to drink.
There are even water bottles that you can sync up with your phone and track your water intake. Add electrolytes to your water for an increased boost of hydration.
Exercises to Combat Leg Cramps
Basic Leg Scissors
Leg scissors are simple exercises you can do at home on the floor. This exercise increases circulation in your legs. It also helps maintain muscle tone in your thighs and lower abdomen. Although it doesn’t burn a lot of calories, it is a great way to reduce nighttime leg cramps. Try doing these daily for at least 15 minutes.
Lie on a mat and relax your back enough to feel the length of your spine against it. With your arms resting on the mat, lift both legs about a foot off the floor.
Raise your right leg slightly higher than the left leg. Then, lower your left leg down to the mat as you raise your right leg three or four inches higher. Repeat lifting and lowering legs if you feel comfortable doing so.
After several weeks of performing leg scissors, try wearing ankle weights for resistance.
Squat Rotations
Squat rotations are another great exercise for the legs. They improve flexibility, keep bones strong, and help prevent injury. Squat rotations are one of the best functional exercises to tone and strengthen the body.
Because of its low impact, this exercise is perfect for people of any age and body type.
You’ll need a light medicine ball or any small, weighted object for this exercise. Stand tall with feet hip-width apart and hold the ball in your hands. Keep your chest up, back flat, and your body weight on your heels.
Twist your torso while bringing the ball down to the outside of your left foot. Stand straight with the force of your heels. Repeat on the right side. Keep your eyes locked on the ball during the entire exercise. Do 10 reps on each side.
Stationary Single Leg Holds
The stationary single leg hold exercise works on every lower body muscle. This includes your glutes, quads, hamstrings, and calves. It’s a low impact exercise and doesn’t put too much pressure on knees or joints. Use a wall for support if you need to.
While keeping your knees close, pull your left leg behind your body with your left hand. Once you feel balanced, lift your right arm overhead. Try to keep as straight you can while holding this position and avoid turning your body to the side. Release and switch legs after 10 counts. Repeat three times on both sides.
Want to give your legs extra care this winter? Contact us at NJVVC today for a free varicose vein screening. Early detection is key to preventing damage caused by vascular disease.