Can Spider Veins Come Back After Treatment?
You’ve seen them before. And now you’re seeing them again! Those pesky, unattractive spider veins.
Perhaps you originally had them around your ankles or on your thighs and you sought treatment.
Now they seem to have reappeared, and you’re asking, can spider veins come back after treatment?
About Spider Veins
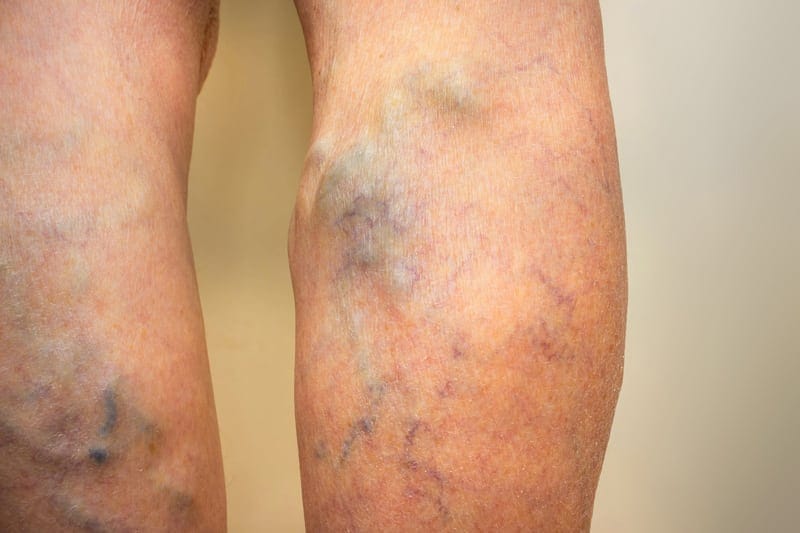
Spider veins are those thin red or blue veins on your skin’s surface.
You will commonly find spider veins on thighs and calves. They also appear on the face and breasts.
Spider veins can be itchy and annoying, or cause legs to feel slightly tired. But they are rarely painful and are almost always harmless.
Today, doctors consider sclerotherapy the best treatment for the removal of spider veins. But this isn’t always the medical procedure performed.

Reasons Spider Veins Return
There are several reasons spider veins return, or at least seem to return.
But what happens most often is that new spider veins develop in the same area after treatment.
So, it’s not that the spider veins that were treated are returning. Rather, new spider veins show up and are mistaken for the original veins.
Reasons spider veins return in the same area include:
- A person has venous insufficiency, so deeper, untreated veins are causing the development of new spider veins
- A person’s body doesn’t properly regulate new vein formation
- The person continues with activities that cause spider veins, such as long periods of sitting or standing, or staying obese
- Saline or skin laser was improperly used to treat them
- Genetics
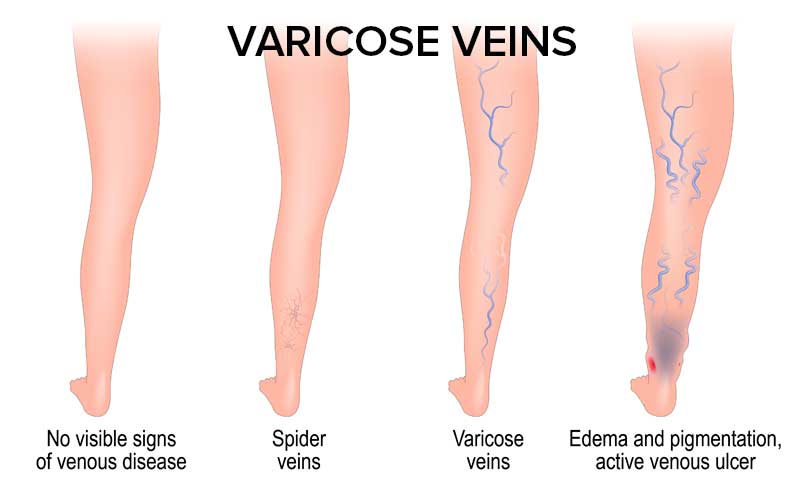
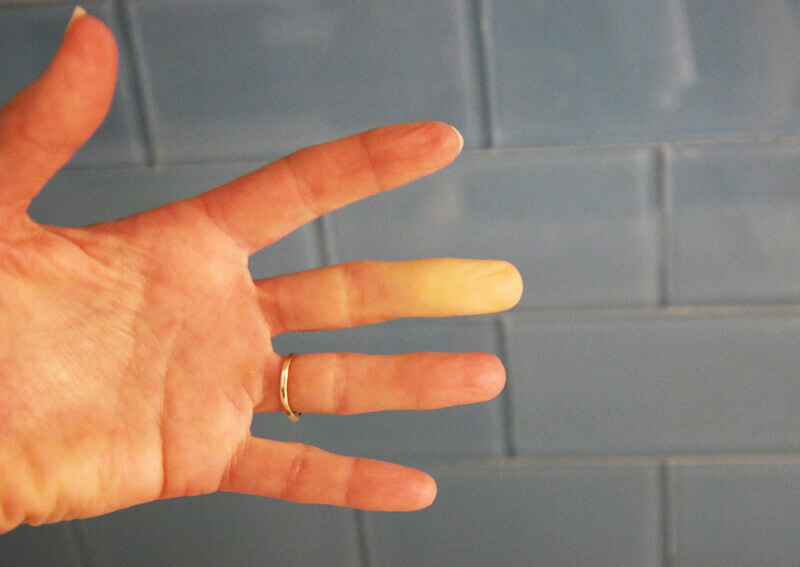
Venous Insufficiency
Venous insufficiency is a progressive vein disease. A vein specialist can treat it, but venous insufficiency will not go away on its own.
If a person has venous insufficiency, the underlying varicose veins combined with an increase in venous pressure encourage the development of new spider veins.
So new spider veins form.
It seems like the old ones are returning, but they’re not.
Doctors can diagnose venous insufficiency with a simple, painless ultrasound of your legs. This will show whether your vein valves are working correctly, and whether you have this condition.
Spider vein treatment should be delayed until this test is performed. If the cause of the spider veins is indeed venous insufficiency, the underlying veins need to be treated first.
If the underlying problem remains untreated, the spider veins are sure to return.
And venous insufficiency needs to be treated for health reasons.
Endovenous laser ablation (EVLT) or Varithena, a micro-foam sclerosant, are favored ways to treat venous insufficiency.
The spider vein won’t be under pressure once the varicose vein receives treatment. At that time, sclerotherapy can treat the spider veins successfully.
If spider veins recur after sclerotherapy, they usually come back in a much less severe form. This happens quite some time after the sclerotherapy procedure.
Genetics and Hormones
If your genetic makeup is encouraging the development of spider veins, trying to get rid of them is an uphill battle.
How do you know your spider veins are caused by genetics?
The easiest way to find out is to ask immediate family members if they’re developing spider veins, too. If they are, you have your answer!
If they aren’t, your spider veins may still be genetic. But the good news is that spider veins caused by genetics are no reason for any health concerns.
Hormonal changes such as pregnancy or menopause can also encourage the development of spider veins.
Laser Therapy
Some doctors use laser therapy as a treatment for spider veins.
Many patients find this procedure to be painful since heat is applied directly to the skin. It also takes a longer time to treat a small area.
Lasers can also cause hypopigmentation—a loss of melanin in the skin.
But most discouraging is that if the laser doesn’t produce enough heat to seal the vein, the procedure will fail. For this reason, you will need additional treatments.
Sclerotherapy
Sclerotherapy is the state-of-the-art treatment for spider veins.
It is considerably more effective and faster than laser treatment. And you don’t feel pain.
During sclerotherapy, the doctor injects a solution or sclerosing agent into the vein.
This causes the vein to scar and collapse. Eventually, you can no longer see the vein since it is resorbed by the body.
Sodium chloride is no longer considered an acceptable sclerosing agent. It can be painful for the patient and can cause serious complications.
Eighty percent of spider veins treated by visual sclerotherapy usually disappear in three to six weeks. So even one treatment of sclerotherapy will create noticeable results.
Patients may need new treatments every few years if new spider veins appear.
How Can You Keep Spider Veins from Recurring?
Are there things you can do after treatment to keep more spider veins from developing?
The answer is yes.
They include:
- Exercising your legs regularly
- Staying at or getting to a healthy weight
- Eating a balanced diet
- Wearing compression stockings or socks
If you want to learn more about spider veins, read:
If you are seeking effective, safe, and comfortable treatment for your spider veins, contact us at NJVVC.