Understanding and Preventing Leg Blood Clots (DVT)
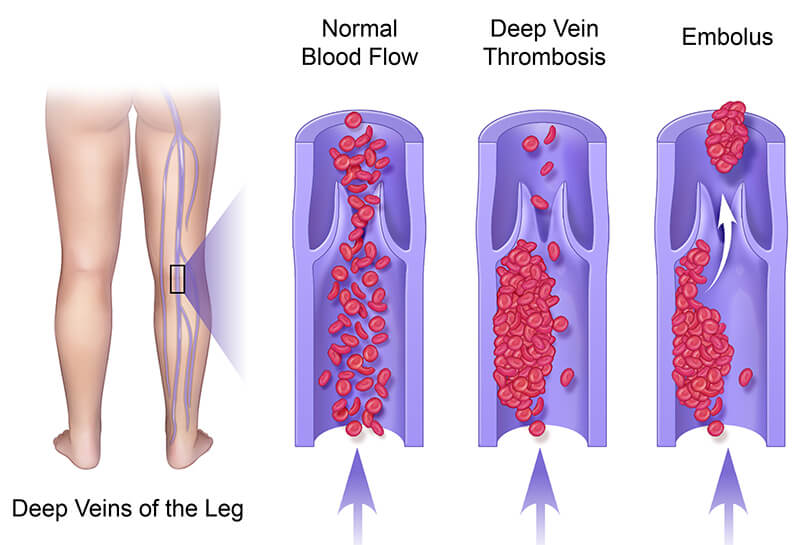
The body has a number of deep veins that circulate blood and return it back to the heart from both legs. However, this phenomenal system also makes legs vulnerable to deep vein thrombosis or DVT.
DVT is a blood clot in the leg. Suffering from a current or repeat blood clot in your leg is not always an instant life-threat, but it can be. In some cases, blood clots can cause the legs to swell or have chronic pain. In other cases, the clot can come loose and cause a lung blockage or cardiac arrest (heart attack).
Deep vein thrombosis isn’t something trivial to ignore, ever. It should be treated, reduced, monitored, and prevented from occurring again.
Where Do Blood Clots Come From?
Deep vein thrombosis occurs when the circulatory system is not able to move blood with enough pressure and regularity. Blood eventually begins to coagulate and clot if it is unable to move around.
A partial slug or clot can start to develop when the body hasn’t moved in a long time, such as in the case of a surgery, a bed-ridden condition, or a long trans-oceanic flight in a cramped seat. Blood clots can even occur in a few hours, as proven in the cases where they are seen in children spending hours playing video games cross-legged.

Common Symptoms of a Blood Clot in the Leg
As blood flow gets blocked or limited, the affected area tends to swell. New blood continues to come in, pumped by the heart, but the returning amount to the heart is less. This creates a backflow or a large amount of pooling in the affected leg.

This pooling effect can be visually noticed by discoloration or an increased amount of heat, similar to an infection or impact location from trauma.
However, many patients have experienced a leg blood clot without any noticeable symptoms. A blood clot’s ability to hide makes them especially dangerous.
Any unusual swelling of the leg, pain, discoloring, or a combination of the above, along with chest pains, dizziness, or inability to breathe, are all signs to receive medical care. Symptoms tend to vary from person to person, so trying to guess if a symptom is serious or not can be a very risky gamble.
Are Blood Clots Genetic?
If a patient’s family has a history of blood-clotting, then it’s quite possible that the patient could be affected as well, studies have proved this. Interestingly, many blood clots are due to lifestyle or changes in mobility.
Obesity or being significantly sedentary for long periods of time will contribute to clotting. If a person is lying down for an extended period due to a surgery or pregnancy, can also be a factor.
Medications that reduce blood pressure have been known to be problematic for clots as well.
How To Prevent Leg Blood Clots or DVT
The easiest and most powerful method of prevention for deep vein thrombosis is to move. Stand up every hour and move your legs around. This will increase circulation and keep blood from pooling. Sitting for extended periods without moving occasionally, such as in an office setting, should be avoided.
Try a convertible desk where you can stand or sit. This will give you options throughout the day. Many companies are now providing them as a low-cost health improvement feature.
If you travel often, walk around the plane frequently or make lots of road stops to walk around and stretch your legs. Again, the hourly changing of position and moving your legs can make a huge difference in preventing leg blood clots or DVT.
Losing weight can significantly increase your internal circulatory power and take a load off your system. Extra weight and fat work against the body, making it harder to move blood through the circulatory network and back up the veins. Getting rid of that excess burden makes it easier for your heart to work and for your circulatory system to be more effective.
A routine of regular exercise is beneficial for your overall health. Optimize your workout and alternate between activities so you’re not bored and static. Move and stretch your body with weight-lifting or aerobic exercise. You don’t need to be the next Olympian; daily exercise with mild effort goes a long way towards improving your blood flow.

Don’t Let a Blood Clot Risk Control Your Life
Again, leg blood clots or DVT can occur for a variety of reasons, not just one thing, like heredity. A person’s lifestyle tends to be a significant contributor to risk. Exercise, a healthy diet, and getting regular doctor checkups all help in preventing DVT and allow for early warning sign detection.
Varicose veins can be an early warning sign of further vein complication and deep vein thrombosis. If you have concerns about the veins in your legs, contact NJVVC for the highest level of patient care.