Jul 27, 2017 | News
What is Restless Leg Syndrome?
Restless Leg Syndrome (RLS), also known as Willis-Ekbom Disease, is a neurological disorder characterized by its overwhelmingly unpleasant urges to move the legs while at rest.

What are the symptoms of Restless Leg Syndrome (RLS)?
Restless Leg Syndrome (RLS) is characterized by its overpoweringly desire to move the legs, particularly while at rest. RLS usually causes leg pain in the evening and night. A common characteristic of RLS is that, in the early morning, legs are typically symptom-free, allowing for a period of better sleep.

Who suffers from Restless Leg Syndrome (RLS)?
While RLS affects about one in ten American adults, it affects almost twice as many women than men.
Is Restless Leg Syndrome (RLS) hereditary?
RLS is not always hereditary, but genetic links have been found in some cases. RLS does seem to run in some families, but not all.

What triggers Restless Leg Syndrome (RLS)?
RLS is most commonly triggered by periods of inactivity. While RLS symptoms seem most prominent at night, the symptoms can appear at any time throughout the day when the legs are inactive. This includes sitting in theaters, on long flights or car trips, or even while relaxing at home.

Are there treatments for Restless Leg Syndrome (RLS)?
Yes! There are a variety of treatment options for dealing with RLS. First, treatment will be directed towards any known underlying illnesses. Prescription medications may be used, such as pain medications, anti-anxiety medications, muscle relaxants, and anticonvulsants. There are also numerous alternative treatment options available such as compression therapy, warm/cold baths, tonic water, oral magnesium, and electric nerve stimulation.

Will my Restless Leg Syndrome (RLS) get worse over time?
Symptoms of Restless Leg Syndrome (RLS) are known to worsen over time. While many experience periods of symptom-free remission, RLS typically re-emerges at some point. Left untreated, RLS symptoms can both worsen and cause other conditions, such as daytime fatigue, depression, travel complications, memory and concentration impairment, insomnia, and exhaustion.
How is Restless Leg Syndrome (RLS) diagnosed?
The National Institutes of Health (NIH) established five specific criteria that must be met for a diagnosis of RLS:
- An overwhelming urge to move the legs, often associated with other unpleasant, uncomfortable, or abnormal sensations.
- The urge to move the legs begins or worsens during periods of rest or inactivity.
- The urge to more the legs is temporarily, partially, or totally relieved by leg movements.
- The urge to move the legs begins or worsens in the evening or night.
- The above symptoms are not due to any other behavioral or medical condition.
For more information about Restless Legs Syndrome and treatment options contact The New Jersey Vein and Vascular Center today!

Jun 29, 2017 | News
A mainly sedentary lifestyle can contribute to the pain and appearance of varicose veins. One of the best ways to improve them is to participate in an exercise program that improves circulation without putting too much stress on your legs and helps with maintaining a healthy weight. Sports and exercising prevent varicose veins so get up and start moving.

Do get out and walk! Walking is probably one of the most important and recommended exercise for varicose vein sufferers, as it is fairly gentle on your legs while promoting circulation. So instead of just grabbing the mail, walk around the block and get your body moving!

Don’t jog or run on hard surfaces. The literal “pounding the pavement” can stress the legs, causing swelling of varicose veins. Instead, try a gentle jog on an even, softer surface such as grass.

Do get in the water! Swimming is a great low-impact exercise that can further develop your calf muscles and aid in improving circulation. This exercise can be done at any level and is great for summer fun.

Don’t participate in high-impact exercise. Heavy weightlifting, while a great workout, can be dangerous for a varicose vein sufferer, as it can put too much strain on the veins of your legs. Using lighter weights with fewer repetitions may be an option if weightlifting is something you love to do. Other such exercises include squats, lunges, and even yoga. Any exercise that increases abdominal pressure can increase leg vein pressure, leading to pain and swelling of varicose veins.

Do get out and bike! Cycling, like walking and swimming, is an ideal low-impact activity that improves circulation while building and strengthening leg muscles. Take a family bike ride in your neighborhood or bring your bike to the park to see more wildlife.

Don’t participate in contact sports. In sports such as football, rugby, and even tennis and skiing. The high probability of injury and sudden, quick movement can be counterproductive to leg vein health.

Starting with walking, cycling, or swimming for 30 minutes a day is a great way to alleviate the pain and appearance of varicose veins.
For more information about your vascular health, contact NJVVC today!

Jun 14, 2017 | News
There are a variety of factors that make a person more susceptible to developing varicose veins. Age, weight, gender, and genetics are some of these, but your occupation may actually be the main culprit of varicose veins. Any job that requires prolonged periods of standing and sitting put you at risk for varicose veins. Some of these occupations include:
- Retail and hospitality
- Healthcare
- Administration and IT
- Hairdressing and barbering
- Truck driving
- Teaching
These are only a few of the examples of the types of jobs that may lead to the development of varicose veins. So, what can be done about it? Fortunately, there are many ways to reduce your risk.

Move!
Exercise is vital in maintaining vascular health by helping to keep weight down and blood flowing. If you work behind a desk all day, try taking a walk on your lunch break or taking the stairs instead of the elevator on your way up to the office.

Kick your heels up
It is also important to rest and elevate your legs when you can. Standing behind a cash register all day can take a toll. Break times should be spent with your legs up whenever possible.

Compression
Compression stockings can aid in keeping blood from pooling in your legs. Commercial drivers may find these especially helpful when time and space are limited.
Taking precautions to prevent varicose veins is crucial. While most of the time they do not cause any long-term medical issues, they can be painful and require surgical intervention. For more information, call a vascular health specialist today.
May 31, 2017 | News
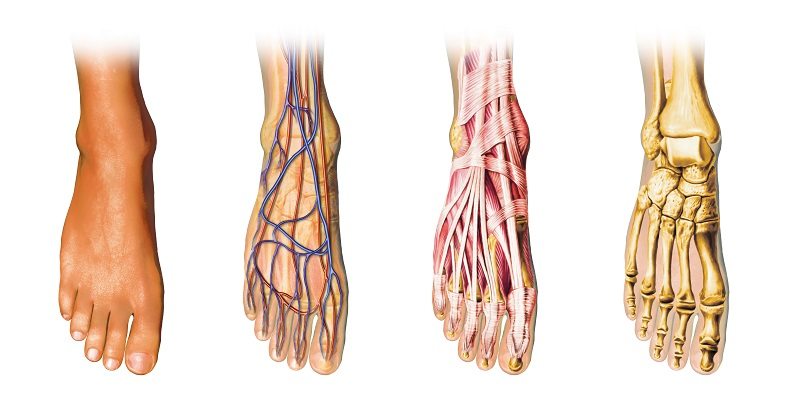
If you are one of the millions of people who suffer from varicose veins or any other circulatory issues, chances are you also suffer from pain and discomfort in your legs, feet, and ankles as well. So, how does poor circulation affect the health of your feet and ankles? Well, Podiatry explains that just like most mechanical things, one small issue somewhere in the body can cause bigger issues elsewhere. Understanding how these things are interconnected can help us stay healthier by way of preventive maintenance.

Chronic Venous Insufficiency
One of the most common circulatory problems that are the source of varicose veins is Chronic Venous Insufficiency (CVI). According to the Society for Vascular Surgery, this condition may affect up to 40% of the United States population, especially women. Patients usually begin to notice symptoms around 50 years of age and above, but it is not unheard of to meet patients suffering from CVI at younger ages as well.

Deep vs Surface Veins
If the affected veins are near your skin, you will notice that the veins in your legs and feet bulge out, look twisted, and are usually a darkish purple color. Sometimes it can look as if you have a bunch of purple grapes bunched up underneath your skin. You may experience your legs and feet feeling achy, tired, or heavy. If the problem veins are closer to the bones, they may not be as obvious, but you will experience chronic swelling in your legs, feet, and ankles, accompanied by aching, tiredness and heaviness in the legs and feet.

Peripheral Artery Disease
Another medical diagnosis for leg and foot discomfort could be Peripheral Artery Disease (PAD). This will cause burning feet due to poor circulation to the area. Peripheral Artery Disease is when the long arteries in your legs become narrower and harder, which in turn limits the blood supply to your legs and feet.

What’s the Damage?
Both CVI and PAD can result in nerve damage in the legs called neuropathy. And though it is statistically proven that around 70% of those with neuropathy suffer from diabetes, there are a number of other factors that can cause leg and foot pain as well. So what can we do to prevent the increase in circulatory problems that result in foot pain? The answer is actually an easy one and costs little to no money: daily exercise.

Become Proactive
Cholesterol and fat are one of the main causes of bad veins (and arteries) due to blockage. When your veins and arteries become clogged due to cholesterol and fat, it becomes more difficult for blood to circulate to and from vital parts or your body (and every part is vital). Exercise also keeps your veins and arteries flexible. This is important because blood pressure can vary depending upon a large number of factors. If your veins and arteries are not elastic enough, this can cause some issues, that in turn may turn into other unforeseeable health problems. Exercise also helps in maintaining a good, healthy weight. Obesity is directly linked to poor circulation and also varicose veins.
For more information of the health of your veins, Contact Us today!

May 23, 2017 | News
Summer is just around the corner which means increased sun exposure is also near! Warnings about the negative effect of too much sun will inevitably pop up all over the internet but, a little sun never hurt anyone, right? Wrong! Many people use the summer sun to get tan and cover up scars, stretch marks, or spider veins but, does that really help? No! Before spending time in the sun this summer, you may want to know more about the negative effects it can have on the amount and appearance of spider veins.
What are spider veins?
Varicose veins are large, visible, raised swollen blood vessels that twist and turn and normally appear in the legs.
Spider veins are smaller, red, purple, and blue vessels that twist and turn. They can be easily seen through the skin and typically present on the legs and face.

What causes spider veins?
Numerous causes affect the appearance of spider veins. They include heredity, obesity, hormonal influence (pregnancy, puberty, menopause), using birth control pills, a history of blood clots, and conditions that cause increased pressure in the abdomen.
How does the sun exposure affect the appearance of spider veins?
The sun exposure plays a role in the development and appearance of spider veins. Ironically, some individuals welcome sun exposure, hoping a nice tan will cover up the veins. Sun exposure may, however, increase the appearance of spider veins specifically around your nose, cheeks, and upper chest.
It’s not just the sun that brings about spider veins. Heat plays a role, too, especially for those with vein disease, a progressive medical condition caused by venous reflux. When elevated temperatures arrive, the body seeks to cool itself. One way it accomplishes this is by dilating and bringing superficial veins (spider veins, for example) to the surface!

What to do about spider veins?
At The New Jersey Vein and Vascular Center we will help you achieve better vein health for a more confident you. See how we can relieve symptoms, prevent complications and improve the appearance of your veins with our minimally invasive techniques for spider vein treatment in NJ. Don’t let another summer pass you by; call today to find out how we can get you feeling comfortable showing off your legs now!
Oct 19, 2016 | News
New Jersey Vein and Vascular Center (NJVVC) proudly announces the launch of our brand new website! The new design is intended to inform and reassure those who suffer from vein conditions that there is hope and exceptional treatment and care available.
We sincerely hope the new website will provide the information needed to understand vein conditions and treatments and recognize that our outpatient treatment for vein conditions is minimally invasive and far less complicated and painful than one would imagine. At NJVVC, the level of quality patient care is state of the art and unparalleled in the North Jersey area.

We focus on the concerns of each individual patient and place great importance on open, comfortable communication and compassion every step of the way.
Many thanks to the Website Design & Development team at Evans Alliance for organizing, coding, and artfully portraying our message.
We welcome you to visit our new website and contact us with any and all questions you may have about your vein condition or symptoms.